Translate this page into:
Key determinants of postmenopausal osteoporosis: A mini-review of current insights

*Corresponding author: Vibhor Joshi, Department of Environmental Biotechnology Genetics and Molecular Biology, National Institute for Research in Environmental Health, Bhopal, Madhya Pradesh, India. vibhorjoshi16@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jogi MK, Sharma R, Rahman A, Aglawe A, Joshi V. Key determinants of postmenopausal osteoporosis: A mini-review of current insights. J Reprod Healthc Med. 2024;5:12. doi: 10.25259/ JRHM_23_2024
Abstract
Osteoporosis, a systemic skeletal disease characterized by low bone mineral density and heightened fracture risk, significantly affects postmenopausal women. This review examines the complex interplay of age, hormonal changes, lifestyle factors, and environmental influences, particularly air pollution, on postmenopausal osteoporosis. With over 200 million individuals impacted globally and an earlier peak incidence in India, there is an urgent need for focused research. This review focuses on estrogen’s crucial role in bone metabolism and how its deficiency leads to increased bone resorption. The adverse effects of air pollution, specifically particulate matter 2.5, on bone health, noting associations between elevated exposure and accelerated bone loss due to inflammation and oxidative stress, were also highlighted. The implications of climate change on osteoporosis risk, particularly regarding fluoride exposure linked to extreme weather patterns, represent a largely underexplored area of research. Explicitly elucidating these multifactorial influences will improve public health policies and promote proactive interventions to reduce osteoporosis risk in postmenopausal women.
Keywords
Postmenopausal osteoporosis
Estrogen
Bone mineral density
Climate change
Pollution
INTRODUCTION
Osteoporosis is a serious health concern that mostly affects elderly people. It is a complicated systemic bone disorder marked by reduced bone mineral density (BMD) and the breakdown of bone architecture that leads to enhanced bone fragility.[1] With ageing, BMD gradually decreases, which can result in primary osteoporosis. This condition predominantly affects women 10– 15 years after menopause and men aged 75–80. As the global population ages, osteoporosis is emerging as a prime health challenge, placing considerable financial pressure on healthcare systems. Research shows that osteoporosis affects over ~200 million people globally.[2] The World Health Organization (WHO) characterizes natural menopause as the permanent end of menstrual cycles lasting at least 12 continuous months without being influenced by any physiological or pathological conditions. Data show that the mean age for normal menopause in developed countries is 51, while in less developed or non-industrialized regions, it typically occurs around the age of 48.[3] With life expectancy reaching approximately 70 years, a large fraction of women will live over 1/3rd of their lives following transition through menopause. Furthermore, the number of women experiencing menopause is rising due to the fast-aging global population. Due to this, ensuring the health and well-being of menopausal women has become a pressing issue worldwide.[4] The WHO data show that osteoporosis affects 30% of women after menopause.[5] In India, around 61 million people are reported to have the condition, with women accounting for 80% of those affected.[6] In India, osteoporosis tends to develop 10–20 years earlier than in Western countries, creating a significant strain on health and economic resources.[7,8] Data on the incidence of postmenopausal osteoporosis (PMO) and the associated risk factors are limited, especially in India, where the condition affects one in three women and one in eight men.[6]
As BMD decreases with advancing age, the prevalence of osteoporosis among women rises significantly. This condition is striking by diminished bone density and an intensified risk of fractures above the age of 50 years, affecting ~1 in three and five in women and men, respectively. The relationship between aging and osteoporosis underscores the importance of monitoring bone health as individuals grow older, particularly since the likelihood of fractures increases with lower BMD levels.[9] The diagnosis of osteoporosis is mainly made through BMD evaluation using X-ray absorptiometry. As per the WHO criteria, osteoporosis and osteopenia are characterized by a T-score of −2.5 or lower and between −1.0 and −2.5, respectively. The femoral neck and lumbar spine are critical anatomical areas for assessing bone health.[5]
FACTORS INVOLVED IN PMO: (AGE, QUALITY OF LIFE, HORMONE, POLLUTION)
Research on osteoporosis generally emphasizes factors such as physical activity, lifestyle, age, chronic stress, environmental factors, and diet [Figure 1]. However, the effects of air pollution on osteoporosis remain largely unexamined. Osteoporosis is a skeletal disorder associated with aging, noticeable by a decrease in bone mass and the weakening of bone microarchitecture, which causes heightened bone fragility. The WHO defines osteoporosis using BMD measurements, describing it as a condition where BMD is 2.5 standard deviations or more below the reference level for an adult.[10] Therefore, BMD is used as a diagnostic marker for osteoporosis. In postmenopausal women and older men, however, BMD consistently drops with age. The risk of osteoporosis-related fractures rises significantly for women over 55 and for men over 65, underscoring the detrimental impact of aging on bone health. Aging influences bone remodeling differently in men and women, resulting in higher rates of bone resorption in women and decreased bone formation and turnover in men.[11] In postmenopausal women, appropriate sleep duration and good sleep quality were positively associated with lower BMD.[12]
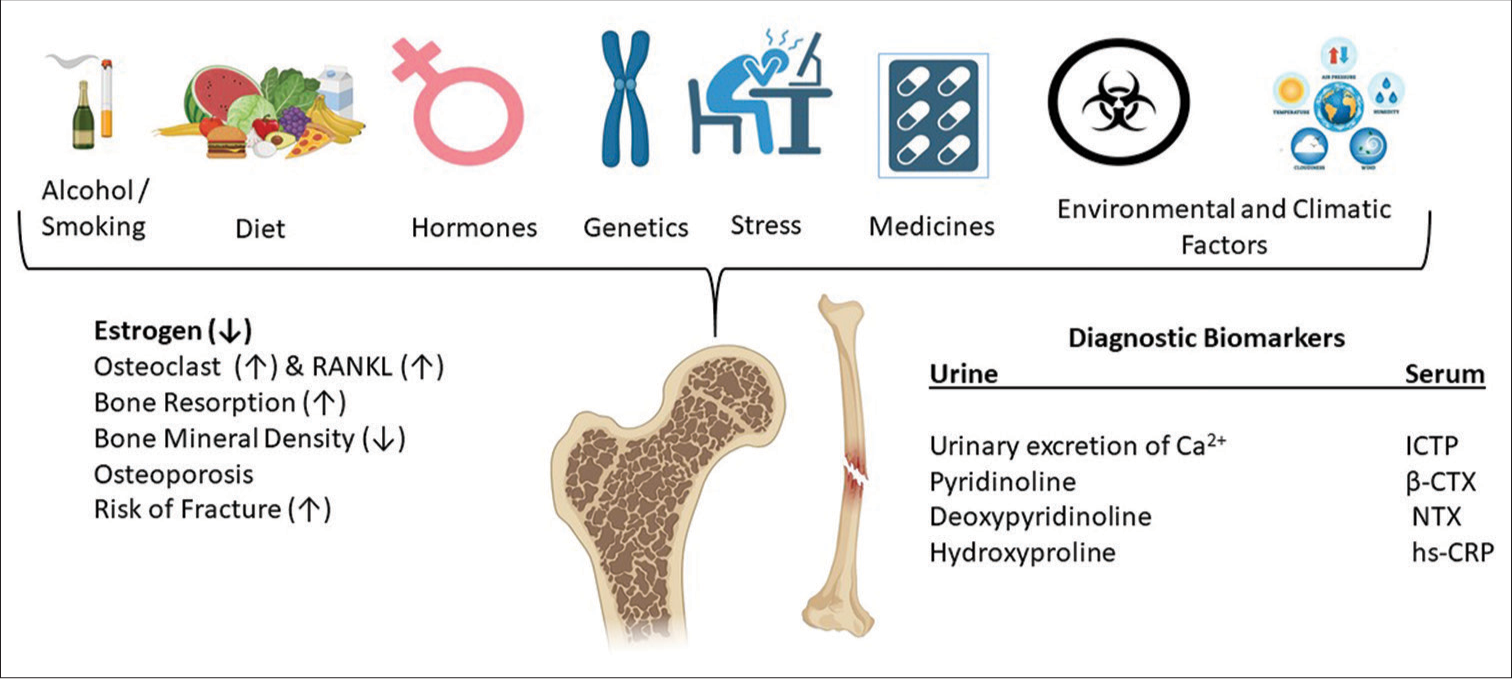
- Role of key molecular determinants (urine and serum-based diagnostic biomarkers) and associated risk factors influencing the progression of osteoporosis in postmenopausal women. The symbols (↑) and (↓) represent upregulation and downregulation, respectively. C-terminal telopeptide of collagen type I, β-CrossLaps, N-terminal telopeptide of collagen type I, and high sensitivity C-reactive protein. ICTP: Cross-linked C-terminal Telopeptide of Type I Collagen, B-CTX: beta-C-terminal telopeptide, NTX: N terminal telopeptide, hs-CRP: High sensitivity C reactive protein.
Hormonal influences on osteoblast and osteoclast metabolism extend beyond sex hormones. Pre-clinical evidence indicates several other hormones, whose levels fluctuate with age, also impact bone metabolism. Increases in cortisol, parathyroid hormone, cortisol, and follicle-stimulating hormone are factors that contribute to bone loss in older adults, whereas decreases in testosterone, vitamin D, insulin-like growth factor 1, and estrogen, testosterone, and vitamin D are factors that contribute to bone mass preservation.[13] Osteoporosis significantly affects women’s quality of life by increasing the risk of fractures, notably at the hip and spine, which can lead to reduced mobility and long-term disability. Nearly half of postmenopausal women experience at least one stereoscopic fracture, resulting in higher mortality rates, diminished quality of life, and an escalating burden on healthcare systems and society.[14] Beyond fractures, osteoporosis also raises the likelihood of chronic pain and dependency. Several factors contribute to the onset of osteoporosis in postmenopausal women, including hormonal changes such as aging, genetic factors, estrogen deficiency, lifestyle choices like smoking, metabolic disorders, and the side effects of certain medications.[15] Osteoporosis is a widespread condition that affects women after menopause and is closely linked to a significant decline in their quality of life.[4] The primary cause of osteoporosis in women is estrogen deficiency, which becomes particularly significant after menopause. In many postmenopausal women, reduced estrogen levels accelerate bone loss by disrupting the equilibrium between bone resorption and formation. Thus, hormonal imbalance, coupled with increased bone turnover, results in a rapid decrease in bone mass, rendering bones more fragile and susceptible to fractures.[16] Besides estrogen deficiency, other contributing factors to this bone deterioration include insufficient calcium intake and reduced physical activity.
Estrogen is vital for bone remodeling, helping to regulate bone resorption and strengthen areas with lower density. During menopause, the decline in estrogen disrupts this balance, accelerating bone loss in vulnerable areas such as the spine and hips and reducing overall bone strength.[17]
By attaching itself to its receptors, estrogen influences bone metabolism by promoting the production of osteoprotegerin (OPG) and reducing the activity of the receptor-activator of nuclear factor kappa-B ligand (RANKL). This action limits the formation of osteoclasts and decreases bone resorption. In addition, estrogen activates the Wnt/b-catenin signaling pathway, which is imperative for bone formation, and enhances bone morphogenetic protein signaling, guiding mesenchymal stem cells toward developing into osteoblasts rather than adipocytes. In the absence of estrogen, pro-inflammatory cytokines (interleukin [IL]-1 and IL-6) and tumor necrosis factor are released more often, contributing to additional bone loss. OPG binding prevents RANKL from attaching to its receptor RANK (receptor activator of nuclear factor kappa-B), which activates osteoclasts.[16,18]
Estrogen regulates the balance between RANKL and OPG by promoting OPG expression, which reduces bone resorption [Figure 1]. Furthermore, estrogen plays a role in regulating bone health, hinders osteoclast differentiation, and stimulates osteoclast apoptosis through the amplified synthesis of transforming growth factor beta. Without sufficient estrogen, RANKL expression is elevated, which stimulates osteoclastogenesis, resulting in enhanced bone resorption and loss of bone density. In addition, the deficiency of estrogen reduces the signaling mechanisms that promote osteoclast cell death, further contributing to the imbalance in bone remodeling.[19]
People residing in elevated stages of particulate matter 2.5 (PM2.5) air pollution are at superior risk of developing osteoporotic fractures. While air pollution is already the leading environmental cause of mortality, recent studies have also associated it with an enhanced risk of osteoporosis, highlighting its impact on bone health. Prolonged exposure to polluted air may accelerate bone loss, particularly in older adults, adding a new aspect to the health risks associated with air quality.[20] Bones are long-term storage sites for heavy metals [cadmium (Cd), mercury, lead, and aluminum], which bind to calcium in the hydroxyapatite matrix. More than 90% of the lead accumulates in bones and teeth in the body, where it can disrupt bone health by lowering vitamin D levels, inhibiting the function of bone-forming osteoblasts, and promoting the action of bone-resorbing osteoclasts. This imbalance accelerates bone loss and increases the frequency of developing osteoporosis. Long-term exposure to these heavy metals can further impair BMD, compounding the incidence of fractures and bone-related disorders.[21,22] A cohort study revealed that increased air pollution accelerates bone loss in postmenopausal women affected by osteoporosis, with the lumbar spine being particularly affected. Nitrogen oxides were found to be especially harmful, causing a rate of bone loss in the lumbar spine that is twice as fast as that caused by normal aging. This pollution exposure was linked to a 1.22% annual decrease in BMD, highlighting the significant impact of environmental factors on bone health in older women.[23] In addition, these factors suggest that air pollution may significantly raise fracture risk in exposed populations (the elderly and those with co-morbid conditions) and potentially increasing their susceptibility to injuries from falls. Enhancing air quality could be crucial in protecting these individuals from additional health complications.
CLIMATE CHANGE RELATED TO PMO
Air pollution and osteoporosis
Atmospheric pressure and its relationship to osteoporosis is an emerging area of interest, particularly concerning air pollution and its effects on bone health. While atmospheric pressure is not directly linked to osteoporosis, environmental factors, notably air quality, influence bone density and fracture incidence at the population stage.[23] This relationship stems from oxidative stress and inflammation caused by air pollutants, which adversely affect bone health. In this regard, earlier studies have confirmed air pollution as the prime threat for osteoporosis and have suggested the correlation between air pollution and bone loss and also the chances of fracture.[24] In older individuals, systemic oxidative damage and inflammation resulting from particulate matter lead to accelerated bone loss besides increasing the risk of bone fractures. Several toxic components of tobacco, like particulate matter, decrease BMD and increase the risk of bone fractures.[24]
In participants from China, longstanding exposure to PM2.5 was related to the reduction in BMD T-score and enhanced chances of osteoporosis.[25] A study in which 9000 women participants contributed to women’s health initiatives supports an association between air pollution, notably poor air quality, and bone damage, independent of lifestyle, socioeconomic, and demographic factors in postmenopausal women.[23] It was shown that BMD is affected primarily by particulate matter and gases, where nitrogen oxide plays a part in damaging bones and, therefore, leads to osteoporosis. As per the statistics, the yearly postmenopausal bone loss was approximately 1.3–1.5% and 1.4% at the lumbar spine and femoral neck, respectively.[26] These findings, together with previous studies, point to an exhilarating research area in the etiology of osteoporosis.[27] Moreover, it has been observed that higher air pollution speeds up bone loss in postmenopausal women due to temperature variations and environmental factors, such as air quality.
Climate change
Climate change is defined by the WHO as sustained variations in temperature and weather patterns.[28] Climate change is a significant global challenge characterized by rising temperatures, increased pollution and sea levels, warmer temperatures, and erratic variations in rainfall.[29,30] The prime reason for this phenomenon is human activity, notably through the release of greenhouse gases, which have a significant effect on ecosystems, weather patterns, and human health.[23,31] Extreme weather events such as heavy rainfall and heat waves have also increased due to climate change, exacerbating pollution problems in urban areas where smog and particulate matter are prevalent.[32] Heightened pollution levels contribute to poor air quality, which can lead to respiratory diseases and cardiovascular problems. In addition, a study revealed that extended experience with air pollutants (Nitrogen oxide NO and Particulate matter PM) is linked to a reduced BMD and enhanced chances of fractures caused by osteoporosis.[33] People exposed to high concentrations of air pollutants had a higher prevalence of osteoporosis, with the consequences being most noticeable in people over the age of 60.[34] The American Heart Association emphasizes that inflammation and oxidative stress are two ways by which exposure to air pollution can hasten coronary atherosclerosis and worsen its consequences.[35,36] Furthermore, research in this area indicates that the inflammatory pathways linked to cardiovascular disease may potentially lead to the progression of osteoporosis.[37] As a result, improving air quality is imperative for reducing the incidence of osteoporosis, highlighting the relationship between environmental factors and public health outcomes.
With respect to the temperature changes, a study showed that contact with the surrounding temperature (~34°C) improves bone health and inhibits osteoporosis-related bone density loss. This effect was associated with modifications in gut flora, which helps postmenopausal women’s bone health.[38] Later, a study conducted in Wuhan, China, discovered a correlation between low temperatures and a higher incidence of osteoporotic fractures, where hospitalization rates for fractures were higher in the winter than in the summer due to lower temperatures exacerbating problems with bone metabolism.[39] For instance, an increase in climatic temperature pushes people to drink more, which could result in consuming more fluoride from groundwater.[40] In this context, thyroid hormone imbalance has also been linked to endemic fluorosis, which can affect peak bone mass acquisition.[41] Bone health and menarche age are related; research indicates a link between delayed menarche and worse bone health as an adult.[42] These findings demonstrate the effect of temperature changes (such as increased heat) on osteoporosis in postmenopausal women.
Air pollution enhances the incidences of osteoporosis and its severe effects, especially in areas with higher traffic concentrations. Asian ethnicity is a well-established established of osteoporosis.[43] A study predicted that over the next few decades, osteoporosis-related bone fractures, particularly hip fractures, will grow 2.28 times throughout Asia, translating into a 1.59-fold rise in healthcare expenditures.[44] Inadvertent exposure to a wide range of pollutants, such as air pollutants, heavy metals, and endocrine disruptors, can lead to the progression of multiple diseases, including neurological disorders, cancer, cardiovascular problems, and reproductive difficulties.[45,46] According to a study done on a cohort of postmenopausal Swedish women, prolonged exposure to extremely low ambient Cd levels can raise the risk of fractures.[47] On the other hand, in high-altitude regions, the sun emits abundant ultraviolet (UV) rays necessary for vitamin D synthesis, which is critical for calcium absorption and required for keeping bones healthy. Despite ample sunlight/UV rays, a study reveals a problem in which Tibetans suffer from vitamin D deficiency. The study examining postmenopausal Tibetan women disclosed concerning statistics of 229 participants, of which 64.2% demonstrated abnormal bone mass, with 54.6% and 9.6% identified with osteopenia and osteoporosis, respectively. These findings underscore the need to comprehend the interaction between altitude, vitamin D concentrations, and skeletal health. Health initiatives targeted at enhancing environmental air quality would result in the prevention of diseases in the world.[43]
CONCLUSION
Understanding the various factors that influence PMO is crucial for the effective prevention and management of this widespread condition. The emerging topic of how environmental factors influence bone health is an exciting area of exploration. Getting a sample of functional bone as an organ presents significant challenges. Developing artificial bone microenvironments offers a promising avenue for advancing our knowledge. These engineered systems can be designed to replicate the biochemical and physical conditions found in human bones, providing a controlled platform for experimentation by simulating different environmental scenarios such as variations in temperature, nutrient concentrations, or physical loading. By examining these factors, we can gain valuable insights into their impact on bone health over time. In addition, hormonal changes, genetic predispositions, nutritional deficiencies, and lifestyle choices significantly influence bone health during and after menopause. By addressing these factors through proactive measures such as diet, exercise, and medical interventions, women can better mitigate their risk of developing osteoporosis. Continued research and awareness are essential to empower women to make informed decisions about their bone health, ultimately leading to improved life quality and well-being in their postmenopausal years.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The pathogenesis, diagnosis, investigation and management of osteoporosis. J Clin Pathol. 2011;64:1042-50.
- [CrossRef] [PubMed] [Google Scholar]
- Sociodemographic factors affecting the disease acceptance in the group of women with postmenopausal osteoporosis. Int J Occup Med Environ Health. 2022;35:273-83.
- [CrossRef] [PubMed] [Google Scholar]
- Lifestyle and dietary factors determine age at natural menopause. J Midlife Health. 2014;5:3-5.
- [CrossRef] [PubMed] [Google Scholar]
- Primary osteoporosis in postmenopausal women. Chronic Dis Transl Med. 2015;1:9-13.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137-41.
- [CrossRef] [PubMed] [Google Scholar]
- Drugs for the management of osteoporosis: A review. Rev Bras Reumatol. 2011;51:365-71, 379-82
- [CrossRef] [Google Scholar]
- Prevalence and predictors of osteoporosis and osteopenia in postmenopausal women of Punjab, India. Int J Environ Res Public Health. 2022;19:2999.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis and fractures in women: The burden of disease. Climacteric. 2022;25:4-10.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis of osteoporosis and assessment of fracture risk. Lancet. 2002;359:1929-36.
- [CrossRef] [PubMed] [Google Scholar]
- Digital oral health biomarkers for early detection of cognitive decline. BMC Public Health. 2023;23:1952.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of the selective estrogen receptor modulators for the treatment of male infertility: A systematic review and meta-analysis. Expert Opin Pharmacother. 2019;20:1517-25.
- [CrossRef] [PubMed] [Google Scholar]
- A broader strategy for osteoporosis interventions. Nat Rev Endocrinol. 2020;16:333-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of osteoporosis in postmenopausal women: The 2021 position statement of The North American Menopause Society. Menopause. 2021;28:973-97.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis due to hormone imbalance: An overview of the effects of estrogen deficiency and glucocorticoid overuse on bone turnover. Int J Mol Sci. 2022;23:1376.
- [CrossRef] [PubMed] [Google Scholar]
- A comprehensive review on postmenopausal osteoporosis in women. Cureus. 2023;15:e48582.
- [CrossRef] [Google Scholar]
- Estrogen receptors in breast and bone: From virtue of remodeling to vileness of metastasis. Oncogene. 2017;36:4527-37.
- [CrossRef] [PubMed] [Google Scholar]
- Postmenopausal osteoporosis. Nat Rev Dis Primers. 2016;2:16069.
- [CrossRef] [PubMed] [Google Scholar]
- The protean toxicities of lead: New chapters in a familiar story. Int J Environ Res Public Health. 2011;8:2593-628.
- [CrossRef] [PubMed] [Google Scholar]
- Air pollution: A largely neglected risk factor for osteoporosis. Lancet Planet Health. 2017;1:e311-2.
- [CrossRef] [PubMed] [Google Scholar]
- Air pollution and decreased bone mineral density among Women's Health Initiative participants. EClinicalMedicine. 2023;57:101864.
- [CrossRef] [PubMed] [Google Scholar]
- Association of air particulate pollution with bone loss over time and bone fracture risk: Analysis of data from two independent studies. Lancet Planet Health. 2017;1:e337-47.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term exposure to air pollution might decrease bone mineral density T-score and increase the prevalence of osteoporosis in Hubei province: Evidence from China Osteoporosis Prevalence Study. Osteoporos Int. 2022;33:2357-68.
- [CrossRef] [PubMed] [Google Scholar]
- Variability of vertebral and femoral postmenopausal bone loss: A longitudinal study. Osteoporos Int. 1996;6:320-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pollution and global health-an agenda for prevention. Environ Health Perspect. 2018;126:084501.
- [CrossRef] [PubMed] [Google Scholar]
- Climate change. Available from: https://www.who.int/health-topics/climate-change [Last accessed on 2024 Sep 26]
- [Google Scholar]
- Impacts of climate change on the fate of contaminants through extreme weather events. Sci Total Environ. 2024;909:168388.
- [CrossRef] [PubMed] [Google Scholar]
- Climate change and respiratory diseases. Eur Respir Rev. 2014;23:161-9.
- [CrossRef] [PubMed] [Google Scholar]
- Climate change and its impact on biodiversity and human welfare. Proc Indian Natl Sci Acad. 2022;88:160-71.
- [CrossRef] [Google Scholar]
- The impact of air pollution on respiratory diseases in an era of climate change: A review of the current evidence. Sci Total Environ. 2023;898:166340.
- [CrossRef] [PubMed] [Google Scholar]
- Association between exposure to fine particulate matter and osteoporosis: A population-based cohort study. Osteoporos Int. 2022;33:169-76.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term air pollution and adverse meteorological factors might elevate the osteoporosis risk among adult Chinese. Front Public Health. 2024;12:1361911.
- [CrossRef] [PubMed] [Google Scholar]
- Air pollution and cardiovascular disease: A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation. 2004;109:2655-71.
- [CrossRef] [PubMed] [Google Scholar]
- Air pollution exposure and cardiovascular disease. Toxicol Res. 2014;30:71-5.
- [CrossRef] [PubMed] [Google Scholar]
- Osteoporosis and cardiovascular disease: A review. Mol Biol Rep. 2023;50:1753-63.
- [CrossRef] [PubMed] [Google Scholar]
- Warmth prevents bone loss through the gut microbiota. Cell Metab. 2020;32:575-90.e7.
- [CrossRef] [PubMed] [Google Scholar]
- Is cold apparent temperature associated with the hospitalizations for osteoporotic fractures in the central areas of Wuhan? A time-series study. Front Public Health. 2022;10:835286.
- [CrossRef] [PubMed] [Google Scholar]
- Skeletal fluorosis in humans: A review of recent progress in the understanding of the disease. Prog Food Nutr Sci. 1986;10:279-314.
- [Google Scholar]
- The influence of thyroid dysfunction on bone metabolism. Thyroid Res. 2014;7:12.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic literature review of factors affecting the timing of menarche: The potential for climate change to impact women's health. Int J Environ Res Public Health. 2020;17:1703.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental air pollution and the risk of osteoporosis and bone fractures. J Prev Med Public Health. 2018;51:215-6.
- [CrossRef] [PubMed] [Google Scholar]
- An updated hip fracture projection in Asia: The Asian federation of osteoporosis societies study. Osteoporos Sarcopenia. 2018;4:16-21.
- [CrossRef] [PubMed] [Google Scholar]
- Reassessment of the lethal London fog of 1952: Novel indicators of acute and chronic consequences of acute exposure to air pollution. Environ Health Perspect. 2001;109(Suppl 3):389-94.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental and health impacts of air pollution: A review. Front Public Health. 2020;8:14.
- [CrossRef] [PubMed] [Google Scholar]
- Association between environmental cadmium exposure and osteoporosis risk in postmenopausal women: A systematic review and meta-analysis. Int J Environ Res Public Health. 2022;20:485.
- [CrossRef] [PubMed] [Google Scholar]






