Engineered immune cell-based therapeutics for female reproductive tract cancers: Advances and future prospects

*Corresponding author: Arpit Bhargava, Faculty of Science, Ram Krishna Dhamarth Foundation University, Bhopal, Madhya Pradesh, India. arpitbhargava08@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nazeer N, Manna R, Shukla S, Patil A, Bhargava A. Engineered immune cell-based therapeutics for female reproductive tract cancers: Advances and future prospects. J Reprod Healthc Med. 2024;5:14. doi: 10.25259/JRHM_24_2024
Abstract
Cancers of the reproductive tract are one of the major causes of deaths in women. The higher rate of mortality among these cancers are mainly due to late stage disease detection and resistance to existing drugs. As research progresses, personalized medicine, which involves tailoring treatments to the unique characteristics of each patient’s tumor, is expected to play a significant role in the future. Engineered immune cells such as engineered dendritic cells, chimeric antigen receptor (CAR) T-cells, and natural killer (NK) cells have emerged as an innovative approach to cure female reproductive tract cancers (FRCs). These engineered immune cells are designed to boost the immune system’s ability to identify and remove cancer cells, offering new therapeutic opportunities for patients with limited treatment options. The present review highlights the applicability of various engineered immune cell-based approaches to treat FRCs. It also outlines the potential of combining nanoparticle-based engineering strategies to further enhance the effectiveness of the existing immune cell strategies through improving the delivery of immune modulators. Overall, the article highlights the promising potential of immune cell engineering to improve the therapeutic outcomes among patients with FRCs.
Keywords
Nanoengineering
Oncology biomarkers
Chimeric antigen receptor-T-cells
Dendritic cells
Natural killer-cells
INTRODUCTION
The female reproductive tract is a multifaceted system that performs various complex processes associated with reproduction, such as producing gametes, regulating hormones, and providing support for fetal development. Each part of the system works in coordination with other and has its own importance; therefore, appropriate functioning of every organ is vital for women’s health.[1] For instance, the vulva refers to the external female genitalia that comprises mons pubis, labia minora, labia majora, clitoris, and vaginal entrance.[2] The mons pubis, a convex accumulation of adipose tissue situated above the pubic bone, becomes adorned with pubic hair during the onset of puberty. Similarly, the labia majora are the bigger, external skin folds that surround the vulva, while the labia minora, being thinner, are internal skin folds that protect the urethra and vaginal entrance. The clitoris, as an intricate organ abundant in sensory nerve endings, plays a crucial role in sexual stimulation and gratification.[3] While, the vaginal entrance, situated anatomically between the urethra and anus, functions as the ingress to the vagina. The internal female reproductive organs comprise the ovaries, uterus, fallopian tubes, cervix, and vagina.[4] Moreover, the ovaries are the primary female reproductive organs that generate ova and secrete hormones such as estrogen and progesterone. Adjacent to the uterus, the ovaries are situated bilaterally. Acting as a conduit between the ovaries and the uterus, the fallopian tubes facilitate the movement of the egg from the ovary to the uterus for fertilization.[5] Furthermore, the uterus is the organ where a fertilized egg implants and develops into a fetus. Comprising three distinct layers, including the outside layer, middle muscle layer, and inner lining that undergoes thickening during the menstrual cycle, the structure is defined. The cervix represents the lower part of the uterus that connects to the vagina, facilitating the passage of sperm and menstrual fluid. In addition, the vagina is an anatomical structure that serves as a conduit connecting the external genitalia to the uterus and functions as the birth canal during childbirth and is also involved in sexual intercourse.[6]
PHYSIOLOGY OF THE FEMALE REPRODUCTIVE SYSTEM
As it is known that the organs (both internal and external) of female reproductive tract works in excellent coordination to facilitate the processes of menstruation and procreation. The reproductive cycle of a woman can be broadly classified within the onset (menarche) and end (menopause) of the menstrual cycle. During menstrual cycle, the cyclical removal of ova occurs from the ovary for the probable fertilization by the male sperm. Normally, the menstrual cycle comprises three primary phases: The menses, proliferative, and secretory phase. The menses phase refers to the process of shedding the uterine lining and usually lasts for a period of 2–7 days. The proliferative phase refers to the period during which the endometrium, or uterine lining, undergoes thickening in anticipation of a potential pregnancy. This phase usually terminates in ovulation, which takes place on day 14 of a 28-day normal menstrual cycle.[7] During the stage of secretory phase, the endometrium undergoes further thickening and organizes itself for a prospective conception. In the absence of fertilization, the menstrual cycle commences again with the onset of menstruation. Similarly, during the phase of ovulation, a mature follicle releases an egg (oocyte) into the fallopian tube. A spike in luteinizing hormone (LH) following the peak of estrogen levels starts this process.[8] The menstrual cycle, ovulation, and maintenance of pregnancy are all dependent on hormones, primarily estrogen and progesterone, which control the female reproductive system. The coordinated action of hormones secreted by the pituitary gland, hypothalamus, and ovaries fine controls the working of the female reproductive system. Furthermore, they engage in collaboration through a feedback loop to control various phases of the reproductive cycle and prime the body for conception. Afterward, the hypothalamus releases a hormone known as gonadotropin-releasing hormone that invigorates the pituitary gland to release the follicle-stimulating hormone (FSH) and LH.[4,9] When it comes to males, FSH works with Sertoli cells in the testes to help sperm production and encourage the growth of ovarian follicles in females. LH causes ovulation and encourages the corpus luteum to make progesterone in females. In males, it encourages the Leydig cells to make testosterone.[10] Moreover, the ovaries serve as the main source of hormone synthesis in females, releasing estrogen and progesterone. In addition, estrogen, which the ovarian follicles produce primarily, stimulates the development of female secondary sexual traits and thickens the uterine lining throughout the menstrual cycle. After ovulation, the corpus luteum secretes progesterone to facilitate the initial phases of pregnancy and prepare the uterus for implantation.[11] In addition, it hinders the secretion of FSH and LH. Furthermore, FSH and LH govern the menstrual cycle by managing the periodic fluctuations in estrogen and progesterone concentrations. During the follicular phase, FSH promotes the growth of follicles and the synthesis of estrogen, resulting in the thickening of the uterine lining.[12] Following that, an increase in LH subsequently stimulates the liberation of the fully developed egg from the ovarian follicle, a process known as ovulation.[13] In the luteal phase, the residual cells of the follicle gather to construct the corpus luteum, which produces progesterone to make the uterus ready for implantation.[14] Failure of implantation leads to a decline in progesterone and estrogen levels, which, in turn, triggers menstruation.[15]
FEMALE REPRODUCTIVE TRACT CANCERS (FRCs)
Reproductive cancers in females include malignant tumors that are formed in the female reproductive organs, including the ovaries, cervix, vagina, uterus, and vulva. Comprehending the unique attributes, factors that increase the likelihood of occurrence, and approaches for addressing each type of reproductive cancer is essential for successful prevention and control.[16] The human papillomavirus (HPV) high-risk strains are primarily responsible for persistent infection in the cervix, the lowest portion of the uterus that attaches to the vagina, which is where cervical cancer originates.[17] Cervical cancer in its initial stages is typically asymptomatic.[18] However, when the illness advances, women may encounter irregular vaginal bleeding, pelvic pain, and heightened vaginal discharge. Regular screenings such as Pap smears and HPV tests are crucial for the early identification and prevention because cervical cancer can be substantially prevented with vaccination and regular screening procedures.[19] Similarly, ovarian cancer, originating in the ovaries, is known for its vague signs such as abdominal distension, pelvic pain, and changes in urine habits, frequently leading to detection in a late stage. Various risk factors for the cancers of ovary include age, family history, and gene mutations, especially in the regions of BRCA1 and BRCA2 genes. Early detection of cancer poses challenges due to multiple causes; hence, treatment typically involves a combination of surgical intervention and chemotherapy.[20] Conversely, uterine cancer, medically referred to as endometrial cancer, originates in the inner lining of the uterus. It is the predominant kind of cancer affecting the female reproductive system and is frequently detected in persons who have gone through menopause.[21] Common symptoms encompass atypical vaginal bleeding, pelvic pain, and discomfort during sexual intercourse.[22] The primary therapy for uterine cancer is surgical removal of the uterus, with a specific approach depending on the stage of the cancer. Furthermore, although less prevalent, vaginal and vulvar malignancies hold considerable importance in their regard. Unusual vaginal bleeding or discharge can be a sign of vaginal cancer, which develops from the walls of the vagina.[23] On the other hand, vulvar cancer develops in the external genitalia and can be characterized by itching, pain, or visible lesions. These sorts are predominantly prevalent among elderly women. In addition, they could be associated with HPV infection. The standard course of treatment usually includes surgical intervention, and in certain instances, radiation therapy may also be employed. Aside from the more prevalent forms, there are also less common reproductive malignancies such as fallopian tube cancer and peritoneal cancer, which are frequently linked to the development of ovarian cancer.[24] Every category of reproductive cancer possesses distinct risk factors and symptoms. This emphasizes the importance of being attentive and detecting a problem early to have successful therapy. Understanding these types of malignancies is crucial for improving outcomes and devising preventive measures for women’s health. Consequently, ongoing research and public health activities prioritize raising awareness, improving early detection tools, and reducing the impact of these diseases[24] [Table 1].
| Type of Cancer | Cause | Risk Factors | Safe or Life-Threatening | References |
|---|---|---|---|---|
| Cervical cancer | Human papillomavirus (HPV) infection | Age (30-50 years), smoking, multiple sexual partners, weakened immune system | Life-threatening | 17 |
| Ovarian cancer | Genetic mutations (e.g., BRCA1, BRCA2), age |
Family history of ovarian cancer, late menopause, nulliparity (never having been pregnant) | Life-threatening | 20 |
| Uterine (endometrial) cancer | Hormonal factors (estrogen exposure) |
Obesity, late menopause, diabetes, family history of endometrial or colon cancer | Life-threatening | 21,22 |
| Vaginal cancer | HPV infection | Age (60+ years), smoking, past des exposure, history of cervical cancer | Life-threatening | 30 |
| Vulvar cancer | HPV infection | Lichen sclerosis, smoking, age (mostly in older women), history of cervical cancer | Life-threatening | 24,25 |
| Fallopian tube cancer | Genetic mutations | Family history of ovarian or breast cancer | Life-threatening | 44, 45 |
| Peritoneal cancer | Often linked to ovarian cancer | Similar risk factors as ovarian cancer | Life-threatening | 80 |
CURRENT TREATMENT APPROACHES AND LIMITATIONS
The management of cancer has conventionally depended on three main modalities: Surgical intervention, chemotherapy, and radiation therapy. Surgery is commonly used to excise tumors and adjacent tissues, offering a possibly curative method for confined cancers.[25] However, its efficacy decreases for late-stage malignancies or those that have spread to other parts of the body. Chemotherapy, a treatment method that employs cytotoxic chemicals to eliminate cancer cells that are dividing rapidly, continues to be a highly utilized alternative for treatment. However, it also leads to notable side effects as it affects normal, healthy cells.[16,26] The drug’s impact on healthy cells results in notable side effects, including nausea, weariness, immunosuppression, skin irritation, and lethargy. Recent developments in cancer treatment have resulted in the creation of focused medicines.[27] These treatments approaches have the objective of enhancing specificity and minimizing side effects. Targeted medicines specifically target molecular markers linked with cancer, therefore reducing harm to healthy cells.[28] While targeted medicines have the potential to enhance outcomes, they may also give rise to enduring side effects that are now being studied. Interestingly, immunotherapy, a therapeutic method that uses body’s own immune system to remove cancer cells, has shown significant potential in the management of many types of cancer. Although immunotherapy can result in long-lasting responses in certain people, not all individuals exhibit a response to this treatment. Moreover, it can lead to immune-related harmful consequences.[29] However, traditional cancer treatments encounter many restrictions despite these progressions. An important obstacle is the variability of malignancies, which results in diverse therapeutic responses.[30] Moreover, the development of resistance to chemotherapy and targeted therapies is a significant challenge, typically necessitating the utilization of numerous treatments to enhance efficacy. Furthermore, considerations such as financial implications, the limited supply, and the requirement for specialist healthcare facilities can impede the accessibility of novel therapies.[20,31] In addition, researchers are currently investigating novel treatments such as stem cell therapy, gene therapy, and natural antioxidants to address the limitations of conventional therapies. Furthermore, stem cell therapy has shown promise in enhancing the process of recuperation. In addition, it demonstrates the potential to diminish the sizes of tumors.[32] However, there are ongoing worries regarding its long-term durability and its potential to cause the development of tumors. Gene therapy aims to rectify genetic abnormalities and bolster the body’s ability to fight against tumors.[33] Nevertheless, it is imperative to tackle the obstacles associated with delivery systems and immunological responses. However, despite the ready availability of natural antioxidants, they often face challenges concerning their absorption and potential toxicity.[34]
IMMUNE CELL ENGINEERING: AN ALTERNATE THERAPEUTIC OPTION
The management of cancer has traditionally relied on several primary modalities, each with its own advantages and limitations. Understanding these options is crucial for evaluating the emerging field of immune cell engineering as an alternative therapeutic strategy. The treatment of cancer often encompasses various modalities, each possessing distinct mechanisms, benefits, and drawbacks [Figure 1]. Surgery frequently serves as the primary treatment for localized tumors, offering the possibility of total excision; nevertheless, its efficacy markedly declines in advanced stages characterized by metastasis. Chemotherapy, a fundamental component of cancer therapy, utilizes cytotoxic chemicals to target rapidly proliferating cells, effectively addressing various malignancies while also causing significant side effects due to harm to normal, healthy cells.[16] Radiation therapy employs high-energy radiation to eradicate cancer cells and is predominantly successful for confined tumors, while it may also damage surrounding healthy tissues. Targeted therapy seeks to engage specific molecular targets linked to cancer, thereby reducing damage to normal cells; however, the absence of appropriate targets may limit its efficacy.[26] Immunotherapy utilizes the body’s immune system to combat cancer and has demonstrated potential in specific instances; however, not all patients exhibit positive responses, and immune-related side effects may arise. Stem cell therapy aims to restore damaged tissues and shows promise in addressing hematological malignancies; yet, apprehensions regarding long-term effects and the possibility for tumorigenesis persist. Gene therapy seeks to rectify genetic anomalies linked to cancer, offering potential for improved immune responses against tumors; yet, obstacles concerning delivery mechanisms and immunological reactions remain. Natural antioxidants seek to mitigate oxidative stress in the body and may provide a less hazardous alternative to traditional medicines; nevertheless, challenges related to absorption and efficacy may restrict their application. Each of these methodologies offers distinct advantages and obstacles that guide the investigation of novel tactics such as immune cell engineering as a potential therapeutic alternative.[27] With an understanding of these traditional approaches and their respective pros and cons, we can now explore immune cell engineering as a promising alternative therapeutic option that seeks to overcome many limitations faced by conventional treatments.
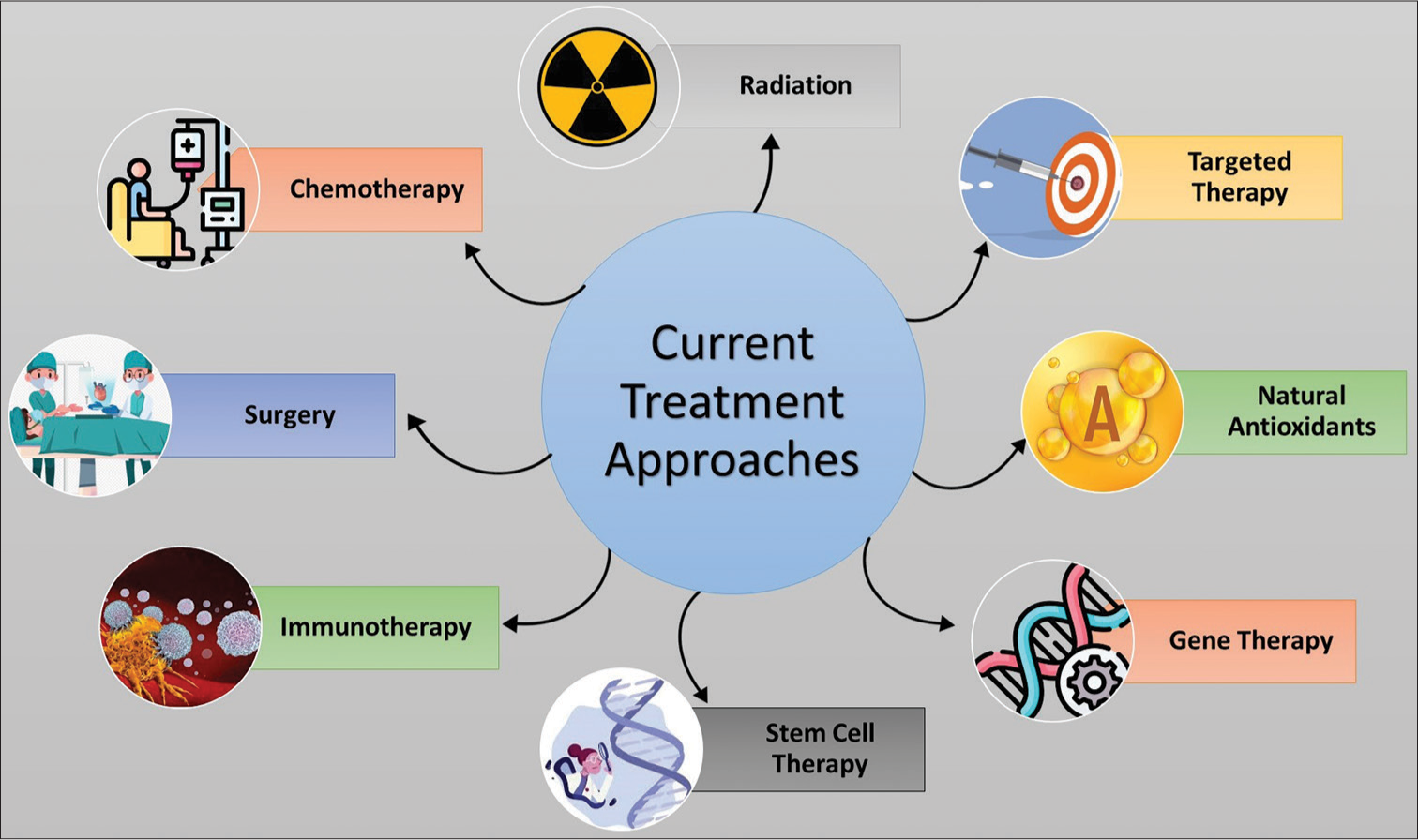
- Image showing different approaches currently used for the treatment of cancer.
The field of cancer immunotherapy has seen substantial transformation with the advancement of immune cell engineering, a technique that harnesses the capabilities of the immune system to detect and eliminate cancer cells. In addition, this novel technique has garnered significant attention due to its capacity to mitigate the limitations of conventional cancer treatments such as chemotherapy and radiation therapy.[35] Furthermore, a key benefit of immune cell engineering is its capacity to selectively target tumor antigens, while limiting any unintended impact on healthy organs. In addition, cancer cells have evolved sophisticated mechanisms to evade or diminish the effectiveness of the immune system, such as downregulating tumor markers or secreting immunosuppressive chemicals.[36] To counteract these, it is proposed to create modified immune cells that can specifically target various antigens, produce cytokines that combat tumors, or interfere with inhibitory pathways. Consequently, this enhances the immune system’s ability to locate and target cancer cells.[37] Furthermore, genetic engineering enables the exact alteration of immune cells to enhance their ability to target tumors and their potential to destroy them through developing chimeric receptors. One such type of cell is chimeric antigen receptor (CAR) T-cells, which are engineered to possess receptors that recognize the antigens specific for tumor cells.[38] Consequently, this enhances their ability to eliminate cancer cells while minimizing the harm to normal cells. This technique has demonstrated exceptional efficacy in the management of hematological malignancies, including acute lymphoblastic leukemia and diffuse large B-cell lymphoma.[30,39] On the other hand, solid tumors provide extra difficulties due to the immunosuppressive environment around the tumor and the absence of appropriate targets, despite the encouraging outcomes observed in blood malignancies.[40] Continue research is underway to find ways that overcome these obstacles and improve the utilization of modified immune cells for the treatment of solid tumors.[41] These endeavors entail modifying immune cells to withstand signals that inhibit the immune system within the tumor microenvironment and identifying novel tumor-specific antigens for precise targeting.[42] Moreover, immune cell engineering can facilitate the development of pre-made treatments in which cells obtained from healthy donors are altered and prepared for quick utilization.[43] In addition, this method can enhance the availability of these treatments to a wider range of patients, as therapies utilizing the patient’s genetically modified T-cells can be laborious and expensive to produce.[43] It is also possible to create modified immune cells that have safety mechanisms, enabling their controlled removal in the event of serious adverse reactions. Modifications can also augment the longevity and expansion of transplanted cells, resulting in more enduring anti-tumor reactions[44] [Figure 2].
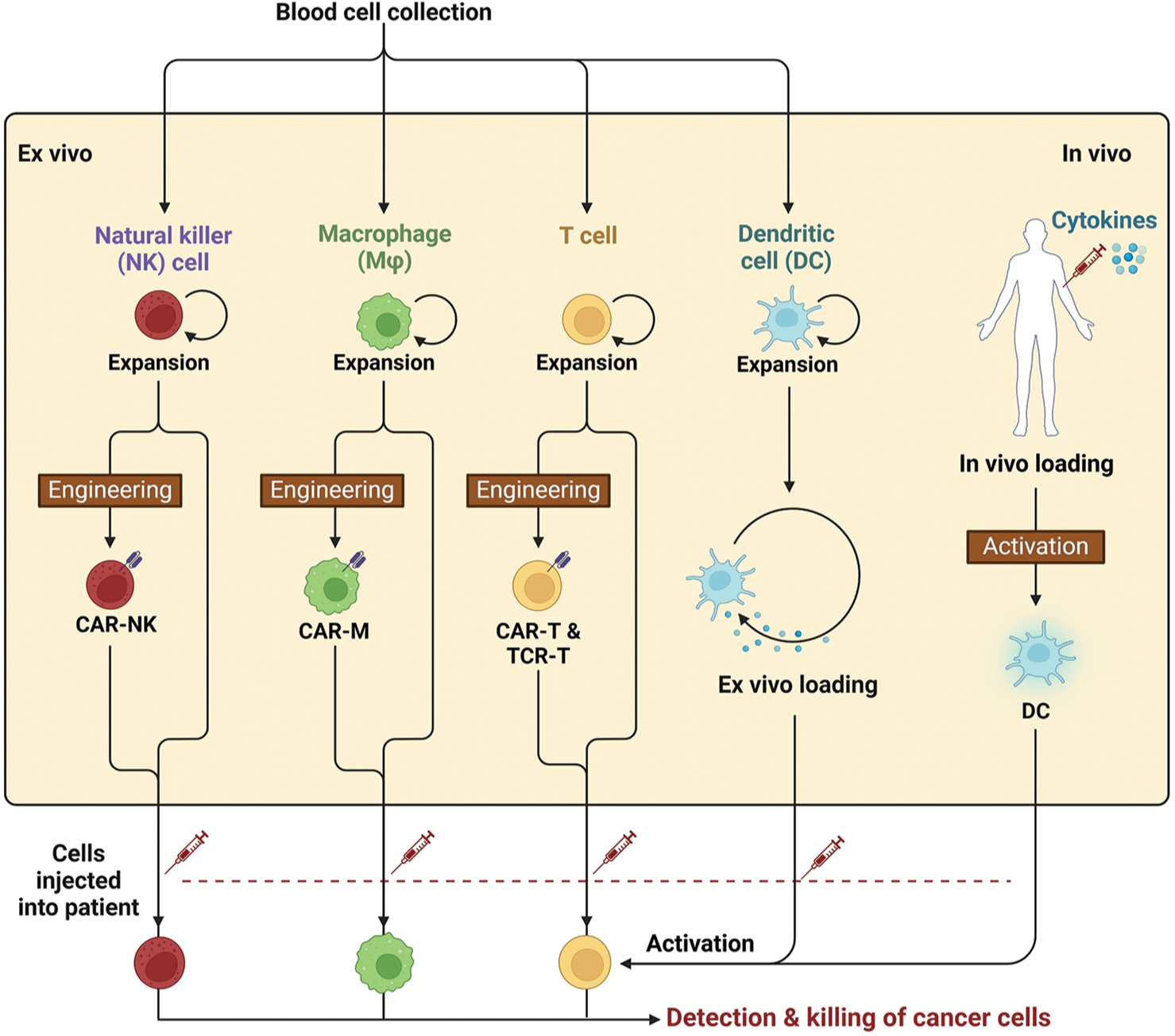
- Image illustrating a brief overview of various stages involved in immune cell engineering, beginning with the collection of blood cells and progressing through the activation of immune cells. This process is crucial for developing effective therapies that enhance the body’s ability to combat diseases like cancer. CAR-NK: Chimeric antigen receptor-Natural Killer cells, CAR-M: Chimeric antigen receptor-Macrophages, CAR-T: Chimeric antigen receptor-T cells, TCR-T: T cell receptor-T cells, DC: Dendritic cells.
Role of immune cells in regulating female reproductive processes
The immune system has an integral role in regulating different process of reproductive tract in women, which importantly includes balancing the protection from pathogens and maintaining tolerance toward sperm and developing embryos.[45] Different types of immune cells, such as natural killer (NK) cells, macrophages, T-cells, and dendritic cells (DCs), perform specific functions that are crucial for reproductive health.[46] Immune cells in the female reproductive system primarily work to maintain immunity against microbial challenges.[46] This is especially important in the lower reproductive tract, which includes the vagina and cervix. Here, immune cells work to prevent infections that could compromise reproductive health.[47] On the other hand, in the upper reproductive tract, including the fallopian tubes and uterus, immune cells need to create a state of immune tolerance to support successful fertilization and embryo implantation. The essential dual function of immune cells underscores their importance in safeguarding against infections and aiding in reproduction.[48] Studies have demonstrated the vital role of NK cells, especially those located in the endometrium, in the menstrual cycle and pregnancy. These cells significantly expand during the late secretory phase of the menstrual cycle and further increase in number during early pregnancy. They help in creating new blood vessels in the endometrial lining, assisting the movement of trophoblasts, and supporting the immune acceptance needed for embryo implantation. The improper functioning of NK cells and other immune cells in the endometrium has been associated with reproductive issues such as infertility and miscarriage. Moreover, T-cells, particularly regulatory T (Treg) cells, have an important role in maintaining immune tolerance during pregnancy. These cells help modulate the immune response to prevent the mother’s immune system from attacking the fetus, which is genetically distinct from the mother.[49] The balance between inflammatory and anti-inflammatory responses is essential for successful implantation and maintenance of pregnancy. Specific molecular pathways involving cytokines and growth factors are responsible for orchestrating inflammation, which is a hallmark of various biological processes such as ovulation, menstruation, and labor. However, the immune system’s involvement in reproductive processes is not without its challenges.[50] For example, excessive activation of immune responses can lead to adverse outcomes such as preterm labor or pregnancy loss. Inflammatory conditions, such as endometriosis, are characterized by elevated levels of certain proteins that cause inflammation, which can disrupt normal reproductive function and contribute to infertility.[16,51]
Immune cell types involved in reproductive processes
Various immune cell types that play crucial roles in both defending against pathogens and preserving reproductive health intricately regulate the female reproductive system. The organs of the female reproductive tract, and hormonal changes throughout the menstrual cycle have an impact on how these immune cells function.[52] For example, NK cells are primarily located in the female reproductive tract, namely, in the endometrium. These cells are of utmost importance throughout the late phase (secretory) of the menstrual cycle and during early pregnancy. These cells contribute to the process of decidual angiogenesis.[53] In addition, they assist in the movement of trophoblast cells and play a role in establishing immunological tolerance. All of these functions are essential for the successful implantation of the embryo. It is essential to increase the number of NK cells in the endometrium to create a supportive environment for the growth of the fetus. An imbalance in these cells has been linked to problems with conception and the occurrence of miscarriages.[54] Similarly, T lymphocytes, comprising CD4 + helper T-cells and CD8 + cytotoxic T-cells, are also present in the female reproductive system. Treg cells, a type of CD4 + T-cells, keep the mother’s immune system from attacking the semi-allogeneic fetus. This is a very important part of maintaining a strong immune tolerance during pregnancy. Ensuring an equilibrium between T-cell responses that stimulate inflammation and those that alleviate inflammation is crucial for the effective establishment and maintenance of implantation and pregnancy.[55] Furthermore, macrophages and DCs also function as immune cells in the female reproductive system, playing a key role in presenting antigens and initiating immunological responses. They perceive and respond to noxious substances while also facilitating the communication between innate and acquired immune responses.[56] These cells maintain a steady environment in the reproductive system by regulating protection against infections and promoting immunological tolerance throughout pregnancy.[57] Apart from this, neutrophils are a distinct category of immune cells that can be detected in the female reproductive system, namely, during the first stages of the menstrual cycle and as a reaction to infections. Neutrophils are the initial responders to infections, rapidly providing defense against pathogens. Mast cells, although less prevalent, also contribute to the immune system in the reproductive tract by producing chemicals that impact inflammation and tissue alterations during the menstrual cycle and pregnancy.[58]
Immune cell function in ovulation, implantation, and pregnancy
Immune cells have important functions in regulating the key reproductive processes, including ovulation, implantation, and pregnancy. Their functions are essential for maintaining reproductive health and ensuring successful outcomes during these critical phases.[59] During ovulation, the immune system plays an active role in the physiological events that result in the release of the oocyte. Immune cells, specifically macrophages, are attracted to the ovarian follicle and assist in the inflammatory reaction that is essential for ovulation.[60] Macrophages assist in the elimination of apoptotic cells and debris, hence aiding in the restructuring of the follicle. Granulosa cells, a component of the ovarian follicle, serve as part of the immune system by producing pro-inflammatory cytokines that are essential for the process of ovulation.[61] The release of LH initiates these immune responses, illustrating the complex interplay between the immunological and endocrine systems in controlling ovulation. After ovulation, the subsequent crucial stage is implantation, during which the fertilized egg must effectively adhere to the uterine lining.[62] Within the endometrium, there is a significant presence of NK cells, which are believed to play a crucial role in the restructuring of blood vessels and the creation of a favorable environment for the successful attachment of the embryo. They regulate trophoblast cells, which are essential for successful implantation and placenta formation.[63] It is essential to maintain a well-balanced immune response during this phase. Excessive inflammation can lead to failure of implantation, whereas a properly regulated immunological response promotes effective attachment and growth of the embryo. During pregnancy, the components of the immune system must adjust to accept the semi-allogeneic fetus while also defending against infections.[64] Treg cells are crucial for creating and upholding this tolerance. Treg cells help suppress the maternal immune response against the fetus, ensuring that the developing embryo is not rejected. In addition, the immune cells secrete specific cytokines and other growth factors that are required for normal development of the fetus.[65] These components are located in the decidua, which is the modified endometrium during pregnancy. If immune cell function is disrupted during this phase, it can result in complications such as preterm labor, miscarriage, or pregnancy-related disorders.[66]
IMMUNE CELL ENGINEERING IN FEMALE REPRODUCTIVE CANCERS
Immune cells have the potential to recognize and attack cancer cells, thereby improving therapeutic outcomes. Utilizing immune cells can transform the treatment of these cancers, often have limited treatment options and poor prognosis.[67] Developing engineered immune cells is one such significant advancement in this field that can better identify and eliminate cancer cells of female reproductive tract. Dr. Coukos’ research at the University of Pennsylvania focuses on developing molecules that increase the ability of immune cell receptors to attach to tumor cells.[68] By engineering these receptors to attach more strongly to ovarian cancer cells, the modified immune cells demonstrate a greater capacity to kill these malignant cells effectively. Early studies in mouse models have shown promising results, indicating that these engineered immune cells could have strong anti-cancer effects in women with advanced ovarian cancer. In addition to ovarian cancer, immune cell engineering is also being explored for other reproductive cancers.[69] As an example, CAR T-cell therapy has been adapted to target specific antigens linked to gynecological tumors. CAR T-cell therapy primarily aims to modify patient’s T-cells to express specific receptors, which can potentially recognize and eradicate cancer cells. The approach has been observed to show potential success in treating hematological malignancies and is now being investigated for solid tumors, including those in the female reproductive system. A study has developed an innovative CAR T-cell therapy targeting the folate receptor alpha, which is overexpressed in ovarian, endometrial, and cervical cancers. Early clinical trials have demonstrated promising results, with some patients experiencing complete remission of their cancer. Furthermore, safety concerns with engineered immune cells have led to the development of advanced systems for better therapy control.[70] A study reports a safety mechanism for CAR T-cells called versatile protease regulatable (VIPER) CAR - T cells, which can be activated or deactivated using an Food and Drug Administration (FDA)-approved antiviral medication. This development aims to reduce the likelihood of severe side effects, like cytokine release syndrome, which may result from the overactivation of engineered T-cells. Furthermore, researchers are investigating the use of ready-made engineered immune cells from healthy donors, which could improve the affordability and availability of these treatments.[71] Despite the potential of immune cell engineering, challenges remain in effectively applying these therapies to solid tumors, including those found in the female reproductive tract. The tumor microenvironment in solid tumors can be immunosuppressive, which makes it challenging for engineered immune cells to function optimally. Ongoing research is focused on overcoming these barriers by improving the persistence and efficacy of engineered immune cells in such environments. Strategies include combining immune cell engineering with other therapies, such as checkpoint inhibitors or targeted drugs, to create a more favorable tumor microenvironment for the engineered cells to thrive in.
Immune cell engineering have emerged as a transformative approach in the treatment of women’s reproductive cancers, including ovarian, cervical, and uterine cancers.[72] This innovative strategy involves modifying immune cells to enhance their ability to recognize and eliminate cancer cells, ultimately improving therapeutic outcomes.[73] Due to advancements in technology and a better understanding of tumor biology, the applications of immune cell engineering in women’s reproductive cancers are numerous and constantly changing.[74] One of the most promising applications of engineered immune cells is in the treatment of ovarian cancer.[75] By creating molecules that bind more tightly to tumor cells, these engineered immune cells demonstrate enhanced cytotoxicity compared to their unmodified counterparts.[76] Early studies in mouse models have shown that these engineered receptors can lead to potent anti-tumor effects, paving the way for potential clinical applications in women with advanced ovarian cancer.[77]
Different approaches of Immune cell engineering
Immunotherapy strategies for FRCs can be broadly classified into three main categories:
DC-based approaches
Lymphocyte-based approaches
CAR T-cell therapy.
DC-based approaches
Using engineered DCs has become an important approach for treating women’s reproductive cancers. It harnesses the unique properties of these antigen-presenting cells to enhance the immune system’s capacity to combat cancers such as ovarian and uterine cancers. DCs play a key role in starting and adjusting the body’s defense mechanisms, making them excellent choices for immunotherapy.[78] DC-based immunotherapy usually involves taking autologous DCs from a patient’s blood, letting them mature, and then loading them with tumor antigens (TSAs/TAAs). The activated DCs are then reinfused into the patient to stimulate a robust anti-tumor immune response. This approach has been explored in several clinical trials, with promising results in various cancers, including gynecological malignancies.[79] For instance, studies have indicated that DC immunotherapy can enhance T-cell responses against uterine cancer, which is often characterized by limited treatment options and a need for novel therapeutic strategies. DC cell-based therapies hold significant promise for treating reproductive cancers, particularly ovarian and uterine cancers. It has been highlighted that DCs can be engineered to target ovarian cancer specific antigens to potentially improve the efficacy of the immune response. Earlier the importance of using a combination of multiple antigens to reduce the risk of immune escape, as tumors often evolve to evade immune detection has been reported.[80] Studies are now exploring how these DC vaccines can be used with other treatments, such as chemotherapy or immune checkpoint inhibitors, to make the whole treatment work better.[81] DC immunotherapy for uterine cancer, the most common pelvic gynecological malignancy, is still in its early stages but shows considerable potential.[82] However, ongoing research aims to identify strategies that can potentially these barriers, as the immunosuppressive tumor microenvironment in uterine cancer poses challenges for effective DC-based therapies. For instance, combining DC vaccines with substances that modify the immune environment may increase the activation and persistence of anti-tumor responses.[83]
Lymphocyte-based approaches
Lymphocyte-based approaches represent a significant advancement in the field of immune cell engineering for the treatment of women’s reproductive cancers, including ovarian, cervical, and uterine cancers. These strategies utilize the special characteristics of white blood cells, specifically T-cells and NK cells.[84] In lymphocyte-based immunotherapy, T-cells or NK cells that can target TAAs are usually activated and made bigger. One effective strategy involves using adoptive cell transfer.[85] This process includes isolating T-cells from a patient, expanding them outside the body, and then reintroducing them to boost the anti-tumor immune response. This approach has demonstrated significant potential in treating a range of cancers, including gynecological malignancies.[86] For instance, tumor-infiltrating lymphocytes (TILs) are T-cells that have entered the tumor environment and have been linked to better survival rates in ovarian and cervical cancers. Research shows that a greater concentration of TILs is linked to improved prognoses, indicating that boosting TIL activity may be a viable treatment approach.[87]
In ovarian cancer, lymphocyte-based approaches are gaining traction due to the tumor’s immunogenicity and the presence of TILs. Research has demonstrated that TILs can be harvested and expanded for therapeutic use, with some clinical trials showing encouraging results in patients with advanced ovarian cancer. Studies are exploring ways to modify T-cells to recognize and attack specific markers present in ovarian cancer. CAR T-cell therapy, successful in blood cancers, is now being tested for effectiveness in solid tumors like ovarian cancer, with promising initial results. In cervical cancer, lymphocyte-based therapies are being explored to enhance the immune response against HPV-associated tumors, including the use of therapeutic vaccines that stimulate T-cell responses against HPV antigens.[88] One approach under investigation involves using therapeutic vaccines to activate T-cells against HPV antigens. In addition, scientists are studying the use of T-cell therapy along with immune checkpoint inhibitors to boost the immune system and improve results for cervical cancer patients. Recent advancements in lymphocyte engineering have focused on improving the specificity and efficacy of T-cells in targeting cancer cells.[89] For instance, the use of cytokine cocktails during T-cell expansion can promote the generation of memory T-cells, which are crucial for long-term anti-tumor immunity.[90] In addition, the combination of TIL therapy with other modalities, such as DC vaccines or immune checkpoint blockade, is being explored to create a synergistic effect that enhances overall treatment efficacy.[91] Another innovative approach involves the engineering of NK cells, which are innate lymphocytes capable of directly killing tumor cells without prior sensitization.[92] NK cell therapy is being investigated for its potential in treating gynecological cancers, particularly due to its ability to target and eliminate tumor cells that may evade T-cell recognition. Advances in genetic engineering techniques, such as clustered regularly interspaced short palindromic repeats/Cas9, are enabling the development of NK cells with enhanced anti-tumor properties, making this a promising area for future research.
CAR T-cell therapy
CAR T-cell therapy is another significant advancement in immune cell engineering, particularly for treating various cancers, including those affecting women.[93] This approach includes modifying the T-cells of patient to express CARs that specifically target antigens present in tumor cells.[94] While CAR T-cell therapy has been observed to possess remarkable effectiveness in hematological malignancies, its application in different types of solid tumors, including ovarian and cervical cancers, is an area of active research.[95] The engineering of CAR T-cells to target specific markers associated with reproductive cancers may provide new therapeutic options for patients who have limited treatment alternatives.[96] The safety of engineered immune cells is a critical consideration in their application for cancer treatment, such as the development of VIPER CAR-T cells, which can be turned “on” or “off ” using FDA-approved antiviral drugs. This system can be controlled and can change the activity of T-cells. This lowers the risk of serious side effects like cytokine release syndrome that are linked to traditional CAR T-cell therapies. Such advancements may enhance the safety and efficacy of immune cell therapies in treating women’s reproductive cancers.[97]
IMPACT OF IMMUNE CELL ENGINEERING ON FERTILITY AND PREGNANCY
The engineering of immune cells have emerged as a transformative approach in the field of reproductive health, with the potential to significantly impact fertility and pregnancy outcomes. Immune cells, including T-cells, NK cells, and DCs, play crucial roles in maintaining reproductive homeostasis, facilitating embryo implantation, and supporting successful pregnancies.[98] However, the manipulation of these immune cells through engineering techniques can have both beneficial and detrimental effects on fertility and pregnancy, necessitating a thorough understanding of their functions and interactions within the reproductive system. Immune cells are integral to various stages of reproduction, including ovarian follicle development, ovulation, and embryo implantation.[99] For instance, uterine NK cells contribute to the remodeling of maternal blood vessels and the establishment of a supportive environment for the implanting embryo. In addition, macrophages and T-cells are involved in regulating the immune tolerance necessary to prevent maternal rejection of the semi-allergenic fetus. The dynamic interactions between these immune cells and reproductive tissues are essential for successful conception and pregnancy maintenance.[100] Research has highlighted the importance of maintaining a delicate balance of immune responses throughout the reproductive cycle, as both excessive inflammation and immune suppression can lead to adverse outcomes.[101] Immune cell engineering, particularly through techniques such as CAR T-cell therapy, has shown promise in enhancing immune responses against tumors.[102] However, the application of these technologies in reproductive health raises important considerations. For example, while engineered T-cells can be designed to target specific cancer cells, their activation can inadvertently disrupt the delicate balance of immune tolerance required during pregnancy.[103] This disruption may lead to complications such as miscarriage or preterm labor. Conversely, the strategic engineering of immune cells could be harnessed to improve fertility outcomes. Increasing the number of Treg cells in the uterine microenvironment has been shown to improve the chances of getting pregnant. This is especially true for women who lose multiple pregnancies or cannot get pregnant due to immune system issues.
LIMITATIONS AND HURDLES
Despite the potential benefits of immune cell engineering in reproductive health, several documented challenges must be addressed:
Complexity of the immune microenvironment
The immunological milieu in the female reproductive system is intricate, requiring meticulously customized therapies to prevent unexpected outcomes. Furthermore, comprehending the interplay between the immune system and reproductive health is essential for formulating effective treatments and interventions.[104]
Risk of fetal rejection
While enhancing NK cell activity may improve anti-tumor responses, it could also increase the risk of fetal rejection if not properly regulated. Therefore, a balance must be struck in therapeutic approaches to ensure both effective cancer treatment and successful pregnancy outcomes. Understanding the delicate immune balance in the reproductive system is essential for optimizing patient care in these complex scenarios.
Long-term effects on fertility and pregnancy outcomes
The prolonged impacts of modified immune cells on fertility and pregnancy results are predominantly uncertain, necessitating comprehensive preclinical and clinical assessment. Furthermore, assessing the effects of immunotherapy on reproductive health in cancer survivors is essential for recognizing potential hazards and formulating suitable therapies. Cooperative endeavors among oncologists, reproductive experts, and immunologists are essential to thoroughly tackle these intricate challenges.[105]
Impact on developing fetus
Researchers must evaluate the implications of immune cell engineering on fetal development, especially if engineered cells or their derivatives are administered during gestation. Comprehending the potential hazards to the developing fetus is essential to guarantee the protection of both the mother and the infant. Researchers must meticulously examine potential detrimental effects and create measures to alleviate them.
Need for standardized protocols
Obstacles persist in the formulation of standardized procedures for DC production and maturation, which are essential for reliable therapeutic results. It is imperative to refine and enhance these methods to guarantee the efficacy and safety of DC-based therapeutics in clinical environments. Collaboration between researchers and regulatory authorities is essential to formulate guidelines that provide consistency and quality control in DC production.[106]
Variability in patient responses
Patient responses to immunotherapy exhibit considerable variability, complicating the formulation of successful treatments. This diversity is attributable to disparities in individual immune systems and tumor microenvironments. Comprehending and resolving these aspects will be essential in enhancing the overall efficacy of immunotherapy treatments.
Immunosuppressive tumor microenvironment
The existence of immunosuppressive factors in the tumor microenvironment presents more hurdles that must be overcome to improve therapeutic success. These variables may impede the immune response and restrict the efficacy of immunotherapy. Research is actively focused on strategies to mitigate immunosuppression within the tumor microenvironment to enhance patient outcomes.[107]
Development of combinatorial strategies
The intricacy of the immune response necessitates novel combinatorial approaches that amalgamate immunotherapeutic approaches with additional therapies to enhance overall effectiveness. This framework enables the explicit presentation of all recorded challenges initially, succeeded by a comprehensive discourse that elaborates on each aspect.[108]
NANOMATERIALS-BASED STRATEGIES FOR IMMUNE CELL ENGINEERING
Nanomaterial’s-based strategies have emerged as innovative solutions in cancer treatment, leveraging the inimitable properties of nanomaterials to enhance therapeutic efficacy, improve drug delivery, and overcome the limitations of conventional therapies.[109] These strategies encompass a varied range of applications, including targeted drug delivery, photothermal therapy (PTT), and gene therapy, and are particularly valuable in addressing the challenges posed by tumor cells such as drug resistance and heterogeneity.[110] Nanomaterials can be engineered to interact with biological systems at the cellular and molecular levels. This allows for the development of nanocarriers that can encapsulate therapeutic agents, such as chemotherapeutics, ribonucleic acid (RNA), or proteins, and deliver them precisely to tumor sites.[111] Nanoparticles can be made to react to certain things, such as changes in pH or the presence of enzymes. This makes it easier to release drugs slowly at the tumor site while minimizing their effects on the rest of the body. Recent advancements have highlighted the use of multifunctional nanosystems that integrate various therapeutic modalities, including photothermal and photodynamic therapies, to enhance the destruction of cancer cells and improve treatment outcomes[112] [Figure 3].
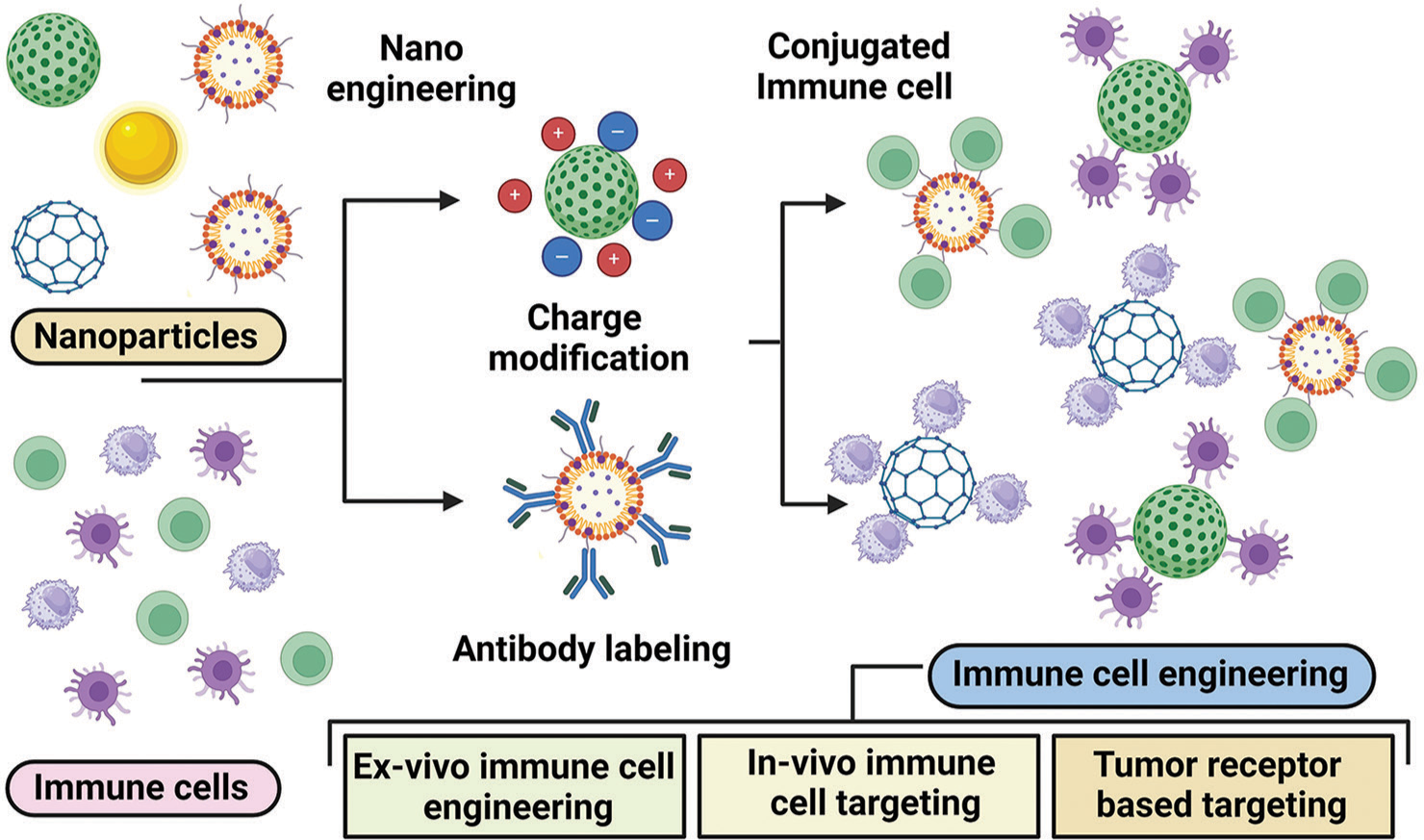
- Image showing the different strategies employed nanoparticles in targeting mechanisms for cancer immunotherapy treatment. This image highlights innovative approaches that increase therapeutic efficacy and specificity, creating the way for more effective cancer treatments.
Nanoparticles can be engineered to target specific tumor markers, allowing for selective delivery of therapeutic agents. This targeted approach reduces off-target effects and enhances the therapeutic index of drugs. For example, gold nanoparticles have been utilized for their ability to enhance the efficacy of radiotherapy through localized heating when exposed to light.[113] Nanomaterials are also being explored as non-viral vectors for gene delivery. They can encapsulate genetic materials such as plasmid deoxyribonucleic acid (DNA), messenger RNA (mRNA), or small interfering RNA (siRNA), facilitating their transport into target cells. This approach is particularly promising for treating genetic disorders and cancers by delivering therapeutic genes that can induce apoptosis in cancer cells or correct genetic defects. Nanomaterials can be employed in PTT and photodynamic therapy (PDT) to selectively destroy cancer cells. In PTT, the involved nanoparticles potentially absorb light and convert it into heat, leading to localized hyperthermia that can kill cancer cells. In PDT, light activates photosensitizers to produce reactive oxygen species, which cause cell death. These techniques can be enhanced using nanomaterials that improve light penetration and retention in tumors, thereby increasing treatment efficacy.[114] Nanomaterials have become integral to the advancement of immune cell engineering, providing innovative approaches to enhance immune responses and improve therapeutic efficacy in various diseases, including cancer. Nanomaterials are useful in immunotherapy because their size, surface area, and ability to be functionalized make it possible to deliver therapeutic agents precisely and control how long they stay in the body. One of the primary applications of nanomaterials in immune cell engineering is the targeted delivery of therapeutic agents to specific immune cells. To selectively target immune cells, we can change the surface properties of nanoparticles and add ligands that bind to specific receptors on those cells.[115] This approach enhances the accumulation of drugs or genetic materials in the desired immune cell populations, thereby increasing therapeutic efficacy while minimizing systemic side effects. For instance, nanoparticles have been designed to deliver immune checkpoint inhibitors directly to T-cells, improving their activation and proliferation in the tumor microenvironment, which is crucial for effective cancer immunotherapy. Nanomaterials also play a significant role in the development of nano-vaccines, which enhance the immunogenicity of antigens. By encapsulating antigens within nanoparticles, these vaccines can protect against degradation and improve stability, ensuring effective delivery to immune cells.[116] In addition, nano-vaccines can co-deliver adjuvants, which further stimulate immune responses. Recent studies have demonstrated that nano-vaccines can effectively activate immune systems, leading to improved protection against tumors and infectious diseases. Nanomaterials can also be engineered to modulate the activity of specific immune cell types. For example, nanoparticles can be designed to activate DCs, enhancing their ability to present antigens and stimulate T-cell responses. This is particularly important in cancer therapy, where effective antigen presentation is crucial for generating robust anti-tumor immunity. In addition, engineered nanoparticles can be used to polarize macrophages toward a pro-inflammatory or anti-inflammatory phenotype, depending on the therapeutic needs, thereby influencing the overall immune response. The ability of nanomaterials to facilitate gene delivery is another critical aspect of their role in immune cell engineering. Nanoparticles can hold different kinds of genetic material, such as plasmid DNA, mRNA, or siRNA.[117] This makes it possible to change immune cells so that they make certain antigens or cytokines. This capability is particularly promising for enhancing the therapeutic potential of immune cells. For example, nanoparticles have been used to send mRNA that encodes tumor antigens to DCs. This causes strong T-cell responses against the tumor. The integration of nanomaterials with other therapeutic modalities, such as immunotherapy and chemotherapy, represents a promising direction in immune cell engineering. By combining nanomaterials with immune checkpoint inhibitors or CAR T-cell therapies, various studies aim to create synergistic effects that enhance overall treatment outcomes. For example, nanoparticles can be used to deliver small-molecule immunomodulators to T-cells, improving their function and persistence in the tumor microenvironment.[118] Moreover, nanoparticles have emerged as promising carriers for the delivery of immune modulators, offering several advantages over conventional delivery methods.[119] By encapsulating or conjugating immune stimulating agents within nanoparticles, the stability, specificity and efficacy of these modulators can be increased with minimal off target effects and targets.[120] This approach has significant implications for the development of more effective vaccines, immunotherapies, and treatments for immune-related disorders. Nanoparticles can protect immune modulators from degradation and clearance, thereby improving their stability and bioavailability.[121] For example, encapsulating cytokines or adjuvants within nanoparticles can shield them from enzymatic degradation and prolong their circulation time in the body. This enhanced stability can lead to more sustained release and prolonged immunomodulatory effects. It can be engineered to target specific immune cell populations, such as DCs, T-cells, or B-cells, by incorporating ligands or antibodies on their surface.[122] This targeted delivery can help immune modulators get into the right cell types more easily, which can make it easier to activate or suppress immune responses. When used in combination with antigens, nanoparticle-delivered immune modulators can enhance the immunogenicity of vaccines. By co-delivering antigens and adjuvants within the same nanoparticle, scientists can create a synergistic effect that promotes antigen presentation, co-stimulation, and the generation of robust, long-lasting immune responses.[123] It can be made to change the way certain types of immune cells work.[124] For example, they can be used to treat autoimmune diseases by encouraging the differentiation of Tregs cells or to treat cancer by making NK cells more effective at killing cancer cells.[125] By delivering cytokines, small molecules, or genetic materials that target key signaling pathways, nanoparticles can fine-tune the activity of immune cells.[126] In the context of cancer immunotherapy, nanoparticles can be used to overcome the immunosuppressive tumor microenvironment. Nanoparticles can strengthen immune systems against tumors by delivering toll-like receptor agonists, immune checkpoint inhibitors, or other immunostimulatory agents.[127] Nanotechnology plays a pivotal role in enhancing immune cell engineering strategies. The nanoparticles deliver immune modulators or antigens directly to immune cells and enhances the activation and proliferation of these cells. Nanoparticles can also enhance the stability and bioavailability of therapeutic agents, allowing for more effective immunotherapy. The integration of nanotechnology with immune cell engineering holds promises for creating more effective and targeted treatments for gynecological cancers. The future of immune cell engineering in women’s reproductive cancers is promising, with ongoing research aimed at optimizing the design and application of engineered immune cells.[128] Advances in understanding tumor microenvironments and immune evasion mechanisms will inform the development of more effective therapies. Furthermore, looking into combination therapies that use immune cell engineering along with other types of treatment, such as radiation and chemotherapy, may have positive effects that help patients do better. Furthermore, personalized medicine approaches, which tailor treatments based on individual tumor characteristics and immune profiles, are likely to play a significant role in the future of immune cell engineering. By leveraging the unique aspects of each patient’s cancer, researchers can develop targeted therapies that maximize efficacy while minimizing adverse effects.[129]
CONCLUSION AND FUTURE PERSPECTIVES
The field of immune cell engineering has recently garnered significant attention as a pioneering approach to combating women’s reproductive cancers. This innovative strategy bolsters the immune system’s capacity to identify and eradicate malignancies, such as ovarian, cervical, and uterine cancers. Engineered immune cells have exhibited promising potential in preclinical and early clinical investigations, encompassing diverse modalities such as CAR T-cell therapy, DC vaccines, and nanoparticle-based delivery systems. These studies have shown significant promise for patients who have limited treatment options. The advancement of this field relies on incorporating cutting-edge technologies and gaining a deep understanding of tumor biology. This is expected to drive the development of more effective and personalized therapies. Exploring combined approaches that involve modifying immune cells and using established treatments such as immunotherapy and chemotherapy shows great potential in overcoming the challenges presented by different types of tumors and immune evasion strategies. In addition, it is essential to implement safety measures in engineered immune cells to ensure patient well-being and minimize side effects. This will facilitate the wider adoption of these therapies in clinical settings. The incorporation of nanotechnology into immune cell engineering further expands the horizons for precise and efficient delivery of therapeutic agents, thereby paving the way for a new era of innovative treatment modalities. In summary, the prospects for immune cell engineering in women’s reproductive cancers are highly optimistic, with the potential to revolutionize the landscape of cancer treatment. To fully realize the potential of these advanced therapeutic strategies, sustained research endeavors and interdisciplinary collaboration among immunologists, oncologists, and engineers will be paramount. As we progress, the steadfast commitment to leveraging the power of the immune system through engineering will play a pivotal role in achieving more effective, personalized, and safer cancer therapies.
CONCLUSION
The engineered immune cell based approaches seems to be promising and further research and trials will certainly provide future treatment options for female reproductive tract cancers.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anatomy and physiology of the uterine cervix. Clin Obstet Gynecol. 2000;43:433-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclic processes in the uterine tubes, endometrium, myometrium, and cervix: pathways and perturbations. Mol Hum Reprod. 2023;29:gaad012.
- [CrossRef] [PubMed] [Google Scholar]
- Organs-on-chip models of the female reproductive system. Bioengineering. 2019;6:103.
- [CrossRef] [PubMed] [Google Scholar]
- Clitoral sexual arousal: neuronal tracing study from the clitoris through the spinal tracts. J Urol. 2008;180:1241-8.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of the female reproductive system: A narrative literature review. Sriwijaya J Obstet Gynecol. 2023;1:16-23.
- [CrossRef] [Google Scholar]
- Physiologic course of female reproductive function: A molecular look into the prologue of life. J Pregnancy. 2015;2015:715735.
- [CrossRef] [PubMed] [Google Scholar]
- Puberty and menstruation knowledge among young adolescents in low-and middle-income countries: A scoping review. Int J Public Health. 2019;64:293-304.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual bleeding, cycle length, and follicular and luteal phase lengths in women without known subfertility: A pooled analysis of three cohorts. Paediatr Perinat Epidemiol. 2020;34:318-27.
- [CrossRef] [PubMed] [Google Scholar]
- Gonadotropin-releasing hormone receptors. Endocr Rev. 2004;25:235-75.
- [CrossRef] [PubMed] [Google Scholar]
- The ovary: Basic biology and clinical implications. J Clin Invest. 2010;120:963-72.
- [CrossRef] [PubMed] [Google Scholar]
- Role of follicle-stimulating hormone in spermatogenesis. Front Endocrinol (Lausanne). 2018;9:763.
- [CrossRef] [PubMed] [Google Scholar]
- Use of follicle-stimulating hormone for the male partner of idiopathic infertile couples in Italy: Results from a multicentre, observational, clinical practice survey. Andrology. 2020;8:637-44.
- [CrossRef] [PubMed] [Google Scholar]
- Luteinizing hormone and its dilemma in ovulation induction. J Hum Reprod Sci. 2011;4:2.
- [CrossRef] [PubMed] [Google Scholar]
- Luteinizing hormone-dependent activity and luteinizing hormone-independent differentiation of rat fetal Leydig cells. Mol Cell Endocrinol. 2001;172:193-202.
- [CrossRef] [PubMed] [Google Scholar]
- Cell biology of leydig cells in the testis. Int Rev Cytol. 2004;233:181-241.
- [CrossRef] [PubMed] [Google Scholar]
- Minerals and the menstrual cycle: Impacts on ovulation and endometrial health. Nutrients. 2024;16:1008.
- [CrossRef] [PubMed] [Google Scholar]
- Age-specific ovarian cancer risks among women with a BRCA1 or BRCA2 mutation. Gynecol Oncol. 2018;150:85-91.
- [CrossRef] [PubMed] [Google Scholar]
- Estrogen-receptor expression and function in female reproductive disease. Cells. 2019;8:1123.
- [CrossRef] [PubMed] [Google Scholar]
- Estrogen biosynthesis and signal transduction in ovarian disease. Front Endocrinol (Lausanne). 2022;13:827032.
- [CrossRef] [PubMed] [Google Scholar]
- Hereditary ovarian cancer and risk reduction. Best Pract Res Clin Obstet Gynaecol. 2017;41:31-48.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of uterine cancer and its management. Expert Rev Anticancer Ther. 2006;6:33-42.
- [CrossRef] [PubMed] [Google Scholar]
- Chemotherapy, radiation, or combination therapy for stage III uterine cancer. Obstet Gynecol. 2019;134:17-29.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of high-risk uterine cancer with whole abdominopelvic radiation therapy. Int J Radiat Oncol Biol Phys. 2000;48:767-78.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar cancer: Epidemiology, clinical presentation, and management options. Int J Womens Health. 2015;7:305-13.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer and radiation therapy: Current advances and future directions. Int J Med Sci. 2012;9:193-9.
- [CrossRef] [PubMed] [Google Scholar]
- New approaches and procedures for cancer treatment: Current perspectives. SAGE Open Med. 2021;9:205031212110343.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer chemotherapy and beyond: Current status, drug candidates, associated risks and progress in targeted therapeutics. Genes Dis. 2023;10:1367-401.
- [CrossRef] [PubMed] [Google Scholar]
- Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct Target Ther. 2018;3:7.
- [CrossRef] [PubMed] [Google Scholar]
- Radiobiology of combining radiotherapy with other cancer treatment modalities In: Radiobiology textbook. Germany: Springer International Publishing; 2023. p. :311-86.
- [CrossRef] [Google Scholar]
- The advantages of using traditional Chinese medicine as an adjunctive therapy in the whole course of cancer treatment instead of only terminal stage of cancer. Biosci Trends. 2015;9:16-34.
- [CrossRef] [PubMed] [Google Scholar]
- Current challenges in cancer treatment. Clin Ther. 2016;38:1551-66.
- [CrossRef] [PubMed] [Google Scholar]
- Prospects for combining targeted and conventional cancer therapy with immunotherapy. Nat Rev Cancer. 2017;17:286-301.
- [CrossRef] [PubMed] [Google Scholar]
- Antiangiogenic therapy: Impact on invasion, disease progression, and metastasis. Nat Rev Clin Oncol. 2011;8:210-21.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell fate in cancer growth, progression and therapy resistance. Nat Rev Cancer. 2018;18:669-80.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering cells for cancer therapy. Acc Chem Res. 2024;57:2358-71.
- [CrossRef] [PubMed] [Google Scholar]
- Advancing cell-based cancer immunotherapy through stem cell engineering. Cell Stem Cell. 2023;30:592-610.
- [CrossRef] [PubMed] [Google Scholar]
- T-Cell engineering for cancer immunotherapy. Cancer J. 2009;15:451-5.
- [CrossRef] [PubMed] [Google Scholar]
- Targeting immune cells for cancer therapy. Redox Biol. 2019;25:101174.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering chimeric antigen receptor-T cells for cancer treatment. Mol Cancer. 2018;17:32.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering approaches for studying immune-tumor cell interactions and immunotherapy. iScience. 2021;24:101985.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering T cells for cancer therapy. Br J Cancer. 2005;93:1085-91.
- [CrossRef] [PubMed] [Google Scholar]
- Role of immune cells and receptors in cancer treatment: An immunotherapeutic approach. Vaccines (Basel). 2022;10:1493.
- [CrossRef] [PubMed] [Google Scholar]
- Strategies to genetically engineer T cells for cancer immunotherapy. Cancer Immunol Immunother. 2016;65:631-49.
- [CrossRef] [PubMed] [Google Scholar]
- Roles of immune microenvironment in the female reproductive maintenance and regulation: Novel insights into the crosstalk of immune cells. Front Immunol. 2023;14:1109122.
- [CrossRef] [PubMed] [Google Scholar]
- The role of sex hormones in immune protection of the female reproductive tract. Nat Rev Immunol. 2015;15:217-30.
- [CrossRef] [PubMed] [Google Scholar]
- Innate immunity in the female reproductive tract: Role of sex hormones in regulating uterine epithelial cell protection against pathogens. Curr Womens Health Rev. 2008;4:102-17.
- [CrossRef] [PubMed] [Google Scholar]
- Hormonal regulation of uterine chemokines and immune cells. Clin Exp Reprod Med. 2011;38:179.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelial cells in the female reproductive tract: A central role as sentinels of immune protection. Am J Reprod Immunol. 2005;53:65-76.
- [CrossRef] [PubMed] [Google Scholar]
- Innate and adaptive immune responses in male and female reproductive tracts in homeostasis and following HIV infection. Cell Mol Immunol. 2014;11:410-27.
- [CrossRef] [PubMed] [Google Scholar]
- Female reproductive system and immunology. Adv Exp Med Biol. 2017;1001:33-57.
- [CrossRef] [PubMed] [Google Scholar]
- Immunology and reproduction In: Yen and Jaffe JaffeJaffe JaffeJaffe Jaffe.3-57.7;100nds:Elsevier. 2019. p. :301-21.e3.
- [CrossRef] [Google Scholar]
- Influence of the immune system on reproductive function. Anim Reprod Sci. 1992;28:171-8.
- [CrossRef] [Google Scholar]
- Evolution of reproductive-immune interactions. Integr Comp Biol. 2006;46:1060-71.
- [CrossRef] [PubMed] [Google Scholar]
- Immune cell type and DNA methylation vary with reproductive status in women: Possible pathways for costs of reproduction. Evol Med Public Health. 2022;10:47-58.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence for the existence and significance of immune cells in male and female reproductive tissues. Immunol Allergy Clin North Am. 1990;10:1-12.
- [CrossRef] [Google Scholar]
- The roles of the immune system in Womenance of immune cells in maley constraints and life history trade-offs. Am J Phys Anthropol. 2011;146:134-54.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokines-involvement in reproduction. Fertil Steril. 1992;58:1093-9.
- [CrossRef] [PubMed] [Google Scholar]
- Endometrial immunity for embryo implantation and pregnancy establishment. Tohoku J Exp Med. 2020;250:49-60.
- [CrossRef] [PubMed] [Google Scholar]
- Human chorionic gonadotropin-mediated immune responses that facilitate embryo implantation and placentation. Front Immunol. 2019;10:2896.
- [CrossRef] [PubMed] [Google Scholar]
- Ovarian and endometrial immunity during the ovarian cycle. J Reprod Immunol. 2019;133:7-14.
- [CrossRef] [PubMed] [Google Scholar]
- Immunology of implantation. Best Pract Res Clin Obstet Gynaecol. 2000;14:827-37.
- [CrossRef] [PubMed] [Google Scholar]
- Immune-like mechanisms in ovulation. Trends Endocrinol Metab. 2008;19:191-6.
- [CrossRef] [PubMed] [Google Scholar]
- Immunoendocrine aspects of endometrial function and implantation. Reproduction. 2007;134:389-404.
- [CrossRef] [PubMed] [Google Scholar]
- Immune regulation of conception and embryo implantation-all about quality control? J Reprod Immunol. 2010;85:51-7.
- [CrossRef] [PubMed] [Google Scholar]
- The immunology of successful pregnancy. Hum Reprod Update. 2003;9:347-57.
- [CrossRef] [PubMed] [Google Scholar]
- Regulation of isocyanate-induced apoptosis, oxidative stress, and inflammation in cultured human neutrophils. Cell Biol Toxicol. 2010;26:279-91.
- [CrossRef] [PubMed] [Google Scholar]
- Collaborative research development grant recipient. 2012. Available from: https://ocrfa.org/grant/program-project-development-grant
- [Google Scholar]
- Epigenetic dimension of oxygen radical injury in spermatogonial epithelial cells. Reprod Toxicol. 2015;52:40-56.
- [CrossRef] [PubMed] [Google Scholar]
- Induction of genomic instability in cultured human colon epithelial cells following exposure to isocyanates. Cell Biol Int. 2009;33:675-83.
- [CrossRef] [PubMed] [Google Scholar]
- Imbalance of mitochondrial-nuclear cross talk in isocyanate mediated pulmonary endothelial cell dysfunction. Redox Biol. 2013;1:163-71.
- [CrossRef] [PubMed] [Google Scholar]
- Nanotechnology in reproductive medicine: Emerging applications of nanomaterials. Nanomedicine. 2014;10:e921-38.
- [CrossRef] [PubMed] [Google Scholar]
- Immunotherapy in cervical and endometrial cancer: Current landscape and future directions. Life. 2024;14:344.
- [CrossRef] [PubMed] [Google Scholar]
- Preconception genome medicine: Current state and future perspectives to improve infertility diagnosis and reproductive and health outcomes based on individual genomic data. Hum Reprod Update. 2021;27:254-79.
- [CrossRef] [PubMed] [Google Scholar]
- Enhanced killing of primary ovarian cancer by retargeting autologous cytokine-induced killer cells with bispecific antibodies: A preclinical study. Clin Cancer Res. 2006;12:1859-67.
- [CrossRef] [PubMed] [Google Scholar]
- Immunotherapy for ovarian cancer: Adjuvant, combination, and neoadjuvant. Front Immunol. 2020;11:577869.
- [CrossRef] [PubMed] [Google Scholar]
- An immunocompetent, orthotopic mouse model of epithelial ovarian cancer utilizing tissue engineered tumor cell sheets. Tissue Eng Part C Methods. 2015;21:23-34.
- [CrossRef] [PubMed] [Google Scholar]
- Immune cell engineering: Opportunities in lung cancer therapeutics. Drug Deliv Transl Res. 2020;10:1203-27.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of tumor antigen-loaded solid lipid nanoparticles as an efficient delivery system for dendritic cell engineering. Nanomedicine. 2013;8:1067-84.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoengineered strategies to optimize dendritic cells for gastrointestinal tumor immunotherapy: From biology to translational medicine. Nanomedicine. 2014;9:2187-202.
- [CrossRef] [PubMed] [Google Scholar]
- Engineered dendritic cellsDCs for gastrointestinal tumor immunotherapy: Opportunities in translational research. J Drug Target. 2013;21:126-36.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative assessment of lipid based nano-carrier systems for dendritic cell based targeting of tumor re-initiating cells in gynecological cancers. Mol Immunol. 2016;79:98-112.
- [CrossRef] [PubMed] [Google Scholar]
- Dendritic cell engineering for tumor immunotherapy: From biology to clinical translation. Immunotherapy. 2012;4:703-18.
- [CrossRef] [PubMed] [Google Scholar]
- Combinatorial strategies for T lymphocyte-based cancer immunotherapy In: Handbook of cancer and immunology. United States: Springer International Publishing; 2022. p. :1-40.
- [CrossRef] [Google Scholar]
- DNA engineered lymphocyte-based homologous targeting artificial antigen-presenting cells for personalized cancer immunotherapy. J Am Chem Soc. 2022;144:7634-45.
- [CrossRef] [PubMed] [Google Scholar]
- Cell-based drug delivery systems participate in the cancer immunity cycle for improved cancer immunotherapy. Small. 2023;19:2205166.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering nano-therapeutics to boost adoptive cell therapy for cancer treatment. Small Methods. 2021;5:e2001191.
- [CrossRef] [PubMed] [Google Scholar]
- Visualization of human T lymphocyte-mediated eradication of cancer cells in vivo. Proc Natl Acad Sci. 2020;117:22910-9.
- [CrossRef] [PubMed] [Google Scholar]
- CAR-T lymphocyte-based cell therapies; mechanistic substantiation, applications and biosafety enhancement with suicide genes: New opportunities to melt side effects. Front Immunol. 2024;15:1333150.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering challenges and opportunities in autologous cellular cancer immunotherapy. J Immunol. 2024;212:188-98.
- [CrossRef] [PubMed] [Google Scholar]
- Cellular immunity augmentation in mainstream oncologic therapy. Cancer Biol Med. 2017;14:121.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer based adoptive T cell therapy. Mol Ther Oncolytics. 2022;24:417-28.
- [CrossRef] [PubMed] [Google Scholar]
- Immunotherapy and immunoengineering for breast cancer; a comprehensive insight into CAR-T cell therapy advancements, challenges and prospects. Cell Oncol. 2022;45:755-77.
- [CrossRef] [PubMed] [Google Scholar]
- Recent findings on chimeric antigen receptor (CAR)-engineered immune cell therapy in solid tumors and hematological malignancies. Stem Cell Res Ther. 2022;13:482.
- [CrossRef] [PubMed] [Google Scholar]
- Emerging CAR-T cell therapy for the treatment of triple-negative breast cancer. Mol Cancer Ther. 2020;19:2409-21.
- [CrossRef] [PubMed] [Google Scholar]
- CAR T cells targeting MISIIR for the treatment of ovarian cancer and other gynecologic malignancies. Mol Ther. 2020;28:548-60.
- [CrossRef] [PubMed] [Google Scholar]
- Artificial engineering of immune cells for improved immunotherapy. Adv Nanobiomed Res. 2021;1:2000081.
- [CrossRef] [Google Scholar]
- Cell therapy in female infertility-related diseases: Emphasis on recurrent miscarriage and repeated implantation failure. Life Sci. 2020;258:118181.
- [CrossRef] [PubMed] [Google Scholar]
- The role of extracellular matrix on unfavorable maternal-fetal interface: Focusing on the function of collagen in human fertility. J Leather Sci Eng. 2022;4:13.
- [CrossRef] [Google Scholar]
- Regulatory T cells improve pregnancy rate in RIF patients after additional IVIG treatment. Syst Biol Reprod Med. 2017;63:350-9.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of immunological response and impacts on fertility following intrauterine vaccination delivered to swine in an artificial insemination dose. Front Immunol. 2020;11:1015.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine natural killer cells: A rising star in human pregnancy regulation. Front Immunol. 2022;13:918550.
- [CrossRef] [PubMed] [Google Scholar]
- Human chorionic gonadotropin as a central regulator of pregnancy immune tolerance. J Immunol. 2013;190:2650-8.
- [CrossRef] [PubMed] [Google Scholar]
- Immune cell hacking: Challenges and clinical approaches to create smarter generations of chimeric antigen receptor T cells. Front Immunol. 2018;9:1717.
- [CrossRef] [PubMed] [Google Scholar]
- Tissue engineering tools for modulation of the immune response. Biotechniques. 2011;51:239-54.
- [CrossRef] [PubMed] [Google Scholar]
- Engineering the next generation of cell-based therapeutics. Nat Rev Drug Discov. 2022;21:655-75.
- [CrossRef] [PubMed] [Google Scholar]
- A photonic dual nano-hybrid assay for detection of cell-free circulating mitochondrial DNA. J Pharm Biomed Anal. 2022;208:114441.
- [CrossRef] [PubMed] [Google Scholar]
- Immuno-cytometric detection of circulating cell free methylated DNA, post-translationally modified histones and micro RNAs using semi-conducting nanocrystals. Talanta. 2021;222:121516.
- [CrossRef] [PubMed] [Google Scholar]
- Quantum dot nanoconjugates for immuno-detection of circulating cell-free miRNAs. Talanta. 2020;208:120486.
- [CrossRef] [PubMed] [Google Scholar]
- Quantum dot based nano-biosensors for detection of circulating cell free miRNAs in lung carcinogenesis: From biology to clinical translation. Front Genet. 2018;9:616.
- [CrossRef] [PubMed] [Google Scholar]
- Cell-free circulating epigenomic signatures: Noninvasive biomarker for cardiovascular and other age-related chronic diseases. Curr Pharm Des. 2017;23:1175-87.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of genetic alterations observed in cell cycle regulatory proteins and microsatellite instability in gallbladder adenocarcinoma: A translational perspective. Asian Pac J Cancer Prev. 2011;12:573-4.
- [Google Scholar]
- Applications of nanoparticles to diagnostics and therapeutics in colorectal cancer. Trends Biotechnol. 2007;25:145-52.
- [CrossRef] [PubMed] [Google Scholar]
- Nanotechnology-based detection and targeted therapy in cancer: Nano-bio paradigms and applications. Cancers (Basel). 2011;3:2888-903.
- [CrossRef] [PubMed] [Google Scholar]
- Engineered nanoparticles: Thrombotic events in cancer. Nanoscale. 2014;6:14141-52.
- [CrossRef] [PubMed] [Google Scholar]
- Nanotechnology for targeted cancer therapy. Expert Rev Anticancer Ther. 2007;7:833-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surface engineering of iron oxide nanoparticles for targeted cancer therapy. Acc Chem Res. 2011;44:853-62.
- [CrossRef] [PubMed] [Google Scholar]
- Tumor targeting strategies of smart fluorescent nanoparticles and their applications in cancer diagnosis and treatment. Adv Mater. 2019;31:e1902409.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoparticle-based approaches to immune tolerance for the treatment of autoimmune diseases. Eur J Immunol. 2018;48:751-6.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoparticle-based nanomedicines to promote cancer immunotherapy: Recent advances and future directions. Small. 2019;15:e1900262.
- [CrossRef] [PubMed] [Google Scholar]
- Advanced strategies in immune modulation of cancer using lipid-based nanoparticles. Front Immunol. 2017;8:69.
- [CrossRef] [PubMed] [Google Scholar]
- Micro and nanoparticle-based delivery systems for vaccine immunotherapy: An immunological and materials perspective. Adv Healthc Mater. 2013;2:72-94.
- [CrossRef] [PubMed] [Google Scholar]
- Harnessing nanoparticles for immune modulation. Trends Immunol. 2015;36:419-27.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoparticle-based drug delivery systems for induction of tolerance and treatment of autoimmune diseases. Front Bioeng Biotechnol. 2022;10:889291.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoparticle-based delivery strategies of multifaceted immunomodulatory RNA for cancer immunotherapy. J Control Release. 2022;343:564-83.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances and challenges of repurposing nanoparticle-based drug delivery systems to enhance cancer immunotherapy. Theranostics. 2019;9:7906-23.
- [CrossRef] [PubMed] [Google Scholar]
- Nanoparticle-based drug delivery systems in cancer: A focus on inflammatory pathways. Semin Cancer Biol. 2022;86:860-72.
- [CrossRef] [PubMed] [Google Scholar]
- Nanotechnology-empowered vaccine delivery for enhancing CD8+ T cells-mediated cellular immunity. Adv Drug Deliv Rev. 2021;176:113889.
- [CrossRef] [PubMed] [Google Scholar]
- Natural killer cells at the forefront of cancer immunotherapy with immune potency, genetic engineering, and nanotechnology. Crit Rev Oncol Hematol. 2024;193:104231.
- [CrossRef] [PubMed] [Google Scholar]







