Translate this page into:
Intrauterine device translocation: Case series and management algorithm

*Corresponding author: Gabriella Argy, Department of Obstetrics and Gynecology, Cipto Mangunkusumo National Hospital, Jakarta, Indonesia. gabyargy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Situmorang H, Argy G, Putri A, Gunardi ER. Intrauterine device translocation: Case series and management algorithm. J Reprod Healthc Med 2022;3:1.
Abstract
Intrauterine devices (IUDs) are the most commonly used long-term contraception due to their 98–99% effectiveness in preventing pregnancy. There are two types of IUD available in Indonesia, a copper-containing IUD and levonorgestrel-releasing IUD. IUD causes chronic inflammatory changes in the endometrium and fallopian tubes that inhibit fertilization and make a hostile environment for implantation. The increased number of endometrial leukocytes is fatal for sperm. In addition, levonorgestrel will inhibit ovulation. The use of an IUD is associated with side effects and complications. The most commonly met complications are IUD expulsion, displacement, translocation, and pregnancy. The average IUD translocation prevalence is 1.3/1000 which mainly occurs during insertion. Translocated IUD may further cause perforation of the bladder or intestines, intestinal obstruction, fistula formation, abscess, adhesion, undesired pregnancy, and chronic pelvic pain. Regardless of the type and location, the WHO recommends removal of the translocated IUD due to its potentially severe complications. Here, we present four cases of IUD translocation at Cipto Mangunkusumo National Hospital from 2020 to 2021, focusing on how to diagnose and the management to remove it.
Keywords
Intrauterine devices
Translocation
Management
Laparoscopy
Hysteroscopy
INTRODUCTION
Intrauterine devices (IUDs) are the most commonly used long-term contraception due to their 98–99% effectiveness in preventing pregnancy.[1] There are two types of IUD available in Indonesia, a copper-containing IUD and levonorgestrel-releasing IUD. IUD causes chronic inflammatory changes in the endometrium and fallopian tubes that inhibit fertilization and make a hostile environment for implantation.[2] The increased number of endometrial leukocytes is fatal for sperm.[3] In addition, levonorgestrel will inhibit ovulation.[1,2]
The use of an IUD is associated with side effects and complications. It has been reported that its most common side effect is vaginal bleeding and the worst complication is uterine perforation.[3] The most commonly met complications are IUD expulsion, displacement, translocation, and pregnancy.[2] The average IUD translocation prevalence is 1.3/1000 which mainly occurs during insertion.[2,3] Translocated IUD may further cause perforation of the bladder or intestines, intestinal obstruction, fistula formation, abscess, adhesion, undesired pregnancy, and chronic pelvic pain.[3] Regardless of the type and location, the WHO recommends the removal of the translocated IUD due to its potentially severe complications.[4]
Here, we present four cases of IUD translocation at Cipto Mangunkusumo National Hospital from 2020 to 2021, focusing on how to diagnose and the management to remove it.
CASE REPORTS
Case 1
A 44-year-old female who was para 4 presented for T-copper IUD evaluation after 1 week of insertion. On anamnesis, the patient admitted that she had pain during defecation. IUD strings were not identified in the physical examination however, the gynecological examination was unremarkable.
On transvaginal ultrasound, the IUD was not identified intrauterine [Figure 1]. On the pelvic radiograph [Figure 2], the IUD was seen at the pelvic region projection. On further evaluation with abdominal CT scan, the IUD was seen at the posterior of the uterus, surrounded by mesenterium fat, anterior to the rectum. The patient underwent laparoscopic removal of the IUD which was identified posterior to the uterus, continued with bilateral tubectomy. The patient recovered well from the surgery.

- Ultrasound showing extrauterine intrauterine devices position.

- X-ray showing the intrauterine devices at the pelvic region projection.
Case 2
A para 1, 21-year-old female presented with a suspected T-copper IUD translocation. The patient had intermittent left abdominal pain that occurred since IUD insertion which was 1 week before the presentation. IUD strings were not identified in the physical examination. On gynecological examination, there was tenderness at the left parametrium.
On the transvaginal ultrasound examination [Figure 3], IUD was identified extrauterine, at the left parametrium, medial to the left ovary. The patient underwent laparoscopic removal of the IUD which was identified at the left mesovarium. The patient recovered well from the surgery and opted for an alternative method of contraception.
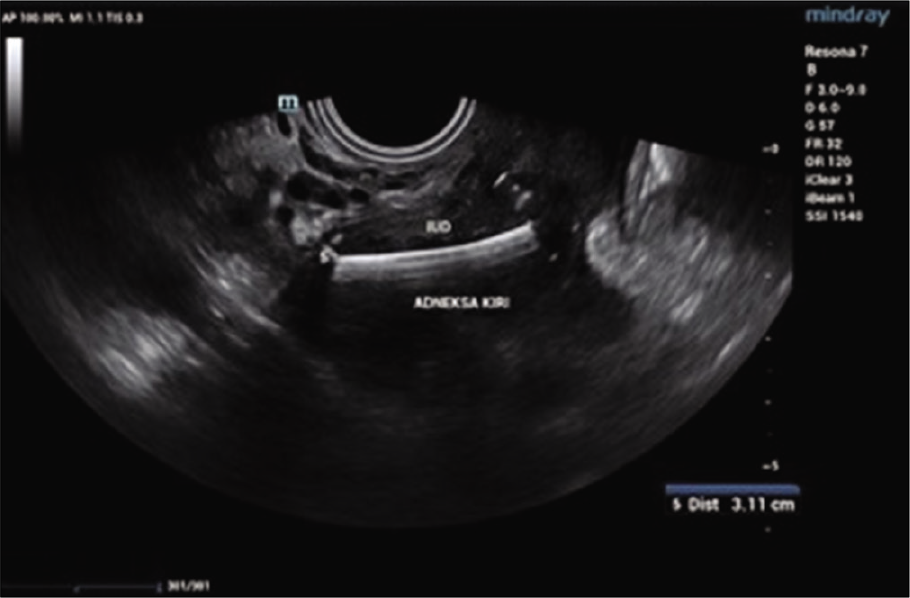
- Ultrasound showing the intrauterine devices at the left adnexa.
Case 3
A para 3, 38-year-old female was referred to our hospital due to translocated levonorgestrel-releasing intrauterine system (LNG-IUS). This patient had been using LNG-IUS for 3 years. She started complaining of back pain 7 months before the examination. On physical examination, the IUD string cannot be identified.
On abdominal x-ray [Figure 4], the IUD was seen at the left paralumbar at the level of L4-5. The patient then underwent laparoscopic IUD removal which was identified at the left mesosigmoid.

- X-ray showing the intrauterine devices at the left paralumbar at the level of L4-5. On abdominal X-ray, the IUD was seen at the left paralumbar at the level of L4-5. The patient then underwent laparoscopic IUD removal which was identified at the left mesosigmoid.
Case 4
A para 1 abortus 1, 33-year-old female presented to our hospital for IUD removal and planned to have a child. She had been complaining about pain during her period for 9 months before the examination. On gynecological examination, the IUD string cannot be identified.
On the ultrasound examination [Figure 5], IUD was identified translocated to the anterior corpus. Hysteroscopy was performed and the IUD was found within the myometrium. The laparoscopic IUD removal was performed. On exploration, a bulging area in the anterior corpus with signs of inflammation was found [Figure 6]. The bulging area was opened and part of the IUD was found protruding from this point [Figure 7]. The IUD was successfully removed. The patient recovered well from the surgery.
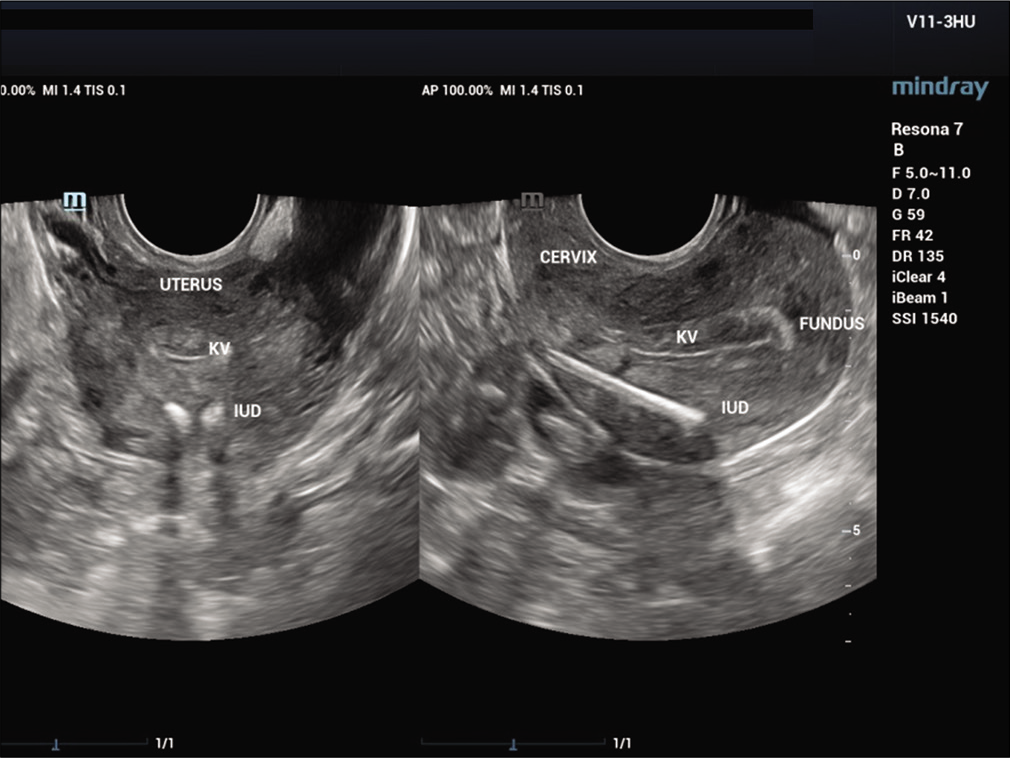
- Ultrasound showing the intrauterine devices was in the myometrium of the anterior corpus.
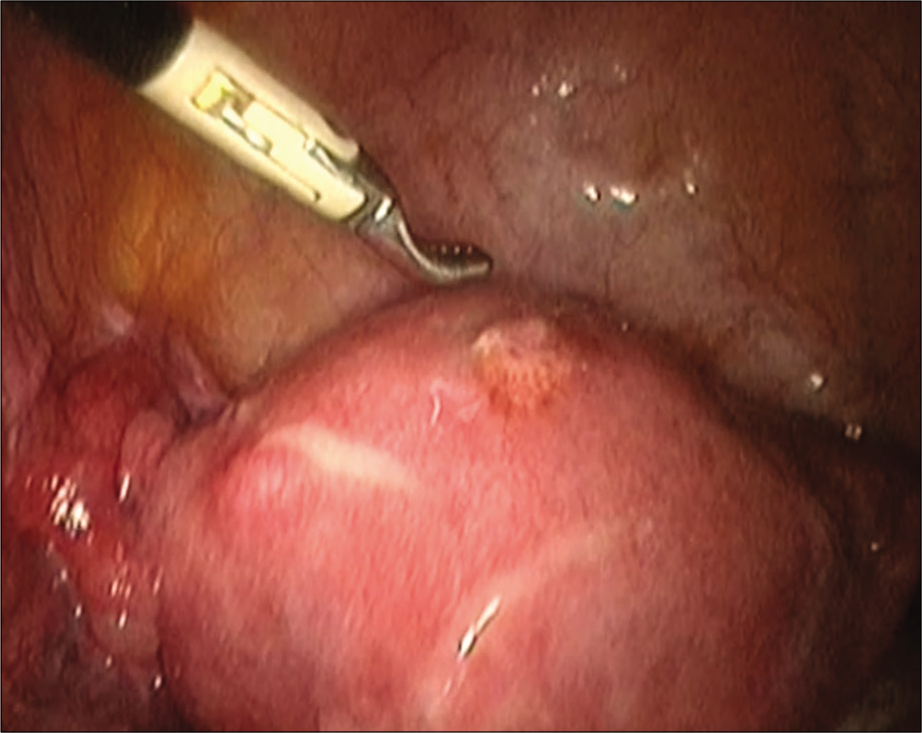
- Laparoscopy showing the bulging area.
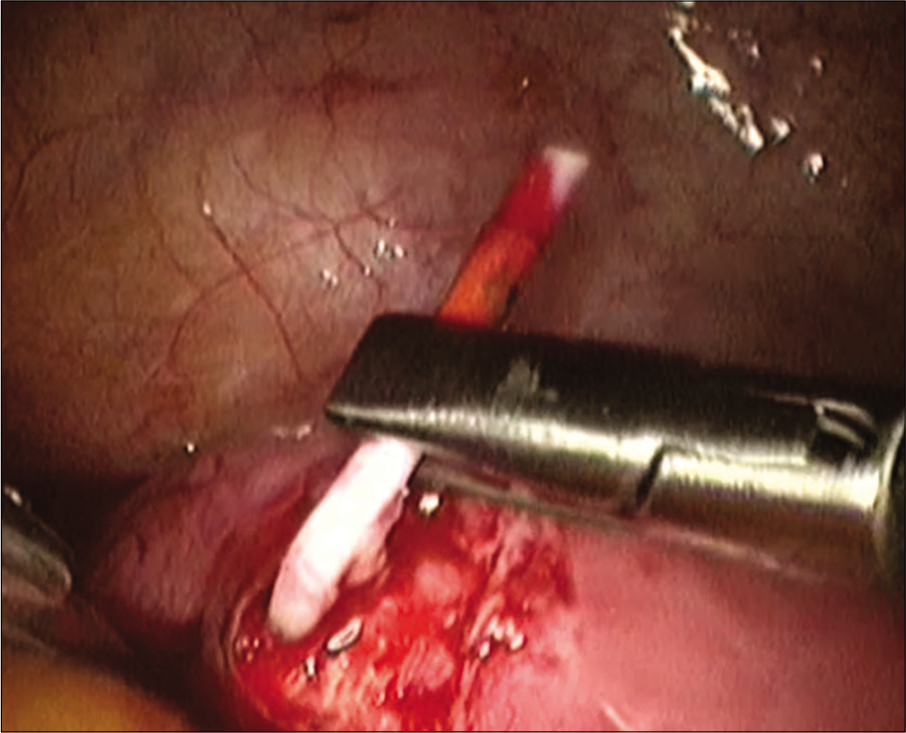
- Intrauterine devices removal on laparoscopic view.
DISCUSSION
Uterine perforation and IUD translocation remain the most harmful IUD complications.[3] However, the prevalence is low, 0.5–13/1000 with an average of 1.3/1000.[2,3] Factors that increase the risk of perforation are insertion by less experienced clinicians, insertion during lactation, nulliparity, poorly healed uterine scar from hematoma or infection, and IUD type.[3,5] Nevertheless, the low prevalence of IUD translocation is due to the renowned withdrawal technique on IUD insertion and the inserter material change into a more flexible type.[5]
IUD translocation happens due to mechanical push on insertion, uterine contraction, and gradual erosion of myometrium.[3,5] Perforation can also happen with uterine sound during uterine cavity measurement.[5] In 90% of patients with uterine perforation is not recognized in the IUD insertion due to its non-specific symptoms.[5] The most common presenting symptoms of IUD translocation are abdominal pain during insertion and after, abnormal uterine bleeding, amenorrhea, dyspareunia, and the most severe is acute abdominal pain.[1-3,5] The symptoms usually lead the patient to visit the clinician, and the most common physical examination result is a non-identifiable on speculum examination.[1,5]
To diagnose IUD translocation, transvaginal ultrasound examination remains superior as the initial study compare to other imaging techniques.[1-3,5] Transvaginal ultrasound is preferred to locate intrauterine IUD.[2,5] Once the IUD is located intrauterine, the clinician may reassure the patient, or remove the IUD at the client’s request. However, when the IUD is found displaced the clinician should examine whether the client has presenting symptoms. In asymptomatic clients, the IUD can remain in place, but if symptomatic, the IUD should be removed using forceps and the procedure is US-guided.
When the IUD is found perforating the myometrium or furtherly perforating all layers of the uterine wall, the clinician should define the exact position and determine the removal technique. We recommend the use of office hysteroscopy to locate the IUD. The partially perforated IUD may be present in one or two, or all three layers of the uterine wall. Type A perforation is mainly located in the uterine cavity than the myometrium.[5,6] In Type D perforation, the IUD lies in all three layers.[6] For Type A and Type D perforation, we suggest a hysteroscopic removal attempt for this type of perforation.
Type B perforation may be a complicated case since most of the device is situated in the myometrium.[6] Furthermore, if the perforation continues, the device can partially pass through the serous layer and protrude into the peritoneal cavity.[6] Laparoscopic removal is recommended for both types of perforation.
With a complete perforation of the device, one may not find the IUD intrauterine on transvaginal ultrasound examination. Full abdominal and pelvic x-ray examination should be ordered to locate the device.[1-3,5,6] Expulsion should be assumed when the IUD does not appear on x-ray examination. However, if the IUD is found in an extrauterine place, the WHO recommends removal irrespective of their location and presenting symptoms.[4] The treatment of choice for complete perforation cases is laparoscopic removal.
Perforating IUD might cause injury to adjacent organs, such as the bowel and bladder.11 The copper elements might contact the recto-sigmoid or the bladder serous layer, resulting in inflammation and causing adhesions.[7,9,11] This process eventually leads to IUD embedment into the lumen.[11]
When the location of the perforated IUD is identified preoperatively, either recto-sigmoid or intravesical, removal using colonoscopy or cystoscopy is a reasonable approach. Otherwise, laparoscopy is the treatment of choice.
LNG-IUS is a newer form of IUD. Based on the operator’s experience, copper IUD translocation was more complicated with adhesion than in the LNG-IUD translocation case. Adhesion is formed due to disturbance in the equilibrium between fibrin deposition and fibrinolytic activity. Fibrinous strands will persist, and will subsequently be infiltrated by proliferating fibroblasts.[7-9] If tissue ischemia exists, an adhesion is created.[7,9] Foreign materials such as translocated IUDs may cause a peritoneal inflammatory reaction. This inflammatory response results in adhesion formation with multiple foreign body granulomas.[7,8]
The effect of progestogens on adhesion formation is still debatable. A retrospective study held in Helsinki found that intra-abdominal adhesions were significantly more common in the Cu-IUD group than in the LNG-IUS group (58 vs. 20%, P = 0.002).[10] On the other hand, a study comparing adhesion formation on IUD and LNG-IUS translocation cases demonstrated no difference in the incidence or severity of adhesions between a perforated copper or LNG-IUD.[8]
Regardless of the type and location, the WHO recommends that all misplaced IUDs should be surgically removed once they are identified.[4] In our study, all displaced IUDs associated with uterine perforation were successfully removed using laparoscopy without significant complications. Laparoscopy has proven a high success rate in the removal of translocated IUDs in patients with uterine perforation.
CONCLUSION
Uterine perforation and IUD translocation are rare complications of IUD insertion, however, pose several morbidities that should be treated on recognition. Transvaginal ultrasound is the preferred initial imaging technique to identify IUD location, followed by an X-ray to locate extrauterine IUD. Once the location of the IUD has been identified, the method of removal may be determined.
Declaration of patient consent
All the patients had been informed and they consented.
Financial support and sponsorship
Nil.
Conflicts of interest
There is no conflict of interest.
References
- IUD embedment in the fallopian tube: An unexpected location for a translocated IUD. Radiol Case Reports. 2018;13:788-92.
- [CrossRef] [PubMed] [Google Scholar]
- Migration of intrauterine devices: Radiologic findings and implications for patient care. Radiographics. 2012;32:335-52.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of predisposing factors, diagnostic and treatment methods in patients with translocation of intrauterine devices. J Obstet Gynaecol Res. 2015;41:735-41.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanism of Action, Safety, and Efficacy of Intrauterine Devices: Report of a WHO Scientific Group Geneva: World Health Organization; 1987.
- [Google Scholar]
- Intrauterine devices and risk of uterine perforation: Current perspectives. Open Access J Contracept. 2016;7:19-32.
- [CrossRef] [PubMed] [Google Scholar]
- Complete and partial perforation and embedding following insertion of intrauterine devices. I Classification, complications, mechanism, incidence, and missing string. Gynecol Surv. 1981;36:335-3.
- [CrossRef] [PubMed] [Google Scholar]
- Peritoneal adhesions: Etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001;18:260-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intraperitoneal levonorgestrel-releasing intrauterine device following uterine perforation: The role of progestins in adhesion formation. Hum Reprod. 2003;18:990-3.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative abdominal adhesions and their prevention in gynecological surgery. Expert consensus position. Gynecol Surg. 2007;4:161-8.
- [CrossRef] [Google Scholar]
- Uterine perforation caused by intrauterine devices: Clinical course and treatment. Hum Reprod. 2013;28:1546-51.
- [CrossRef] [PubMed] [Google Scholar]
- Case report: Ileal perforation after intrauterine device insertion. Open Med. 2021;2:35-7.
- [CrossRef] [Google Scholar]


![Algorithm for intrauterine devices translocation management.[5,6,11] (Modification from Rowlands S, Oloto E, Horwell D. Intrauterine devices and risk of uterine perforation: current perspectives. Open Access J Contracept. 2016).](/content/117/2022/3/1/img/JRHM-3-1-g008.png)




