Translate this page into:
Outcome of intrauterine insemination in couples with unexplained or male factor infertility at National Referral Hospital of Bhutan

*Corresponding author: Gyem Dorji, Department of Anatomy, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan. gyemanatomy@kgumsb.edu.bt
-
Received: ,
Accepted: ,
How to cite this article: Dorji G, Wetasin K, Gyeltshen N, Dorji M. Outcome of intrauterine insemination in couples with unexplained or male factor infertility at National Referral Hospital of Bhutan. J Reprod Healthc Med. 2024;5:1. doi: 10.25259/JRHM_24_2023
Abstract
Objectives:
Jigme Dorji Wangchuck National Referral Hospital (JDWNRH) is the only facility offering intrauterine insemination (IUI) services in the country. In this study, we aim to study the success rate of IUI for the year 2022.
Material and Methods:
This retrospective study utilized secondary data extracted from the medical records of a cohort of 57 patients who underwent IUI procedures at the infertility clinic between January and December 2022. Ethical clearance and site approval were obtained from the Institutional Review Board at Khesar Gyalpo University of Medical Sciences of Bhutan and JDWNRH, respectively. The Statistical Package for the Social Sciences version 26.0 by IBM Corp in Armonk, NY, was used to calculate frequencies, percentages and create statistical diagrams.
Results:
In the year 2022, the overall success rate of IUI was 5.3%. A majority of infertile men, representing 78.9%, fell within the age range of 30–39 years, and oligozoospermia emerged as the most common semen abnormality, affecting 45.6% of the infertile men in this study.
Conclusion:
Our study revealed that the IUI success rate in the country was 5.3%. This success rate of IUI in the country was found to be low compared to the success rate in neighboring countries. This is important information for patients to make informed decisions, aids fertility specialists in devising treatment plans, directs the allocation of resources, drives research and development initiatives, and informs policy and strategic adjustments at the national level.
Keywords
Infertility
Intrauterine insemination
Outcome
Semen parameters
INTRODUCTION
Infertility is defined as the inability of couples to achieve conception after 12 months or more of regular unprotected intercourse.[1] This condition affects approximately 10–15% of couples worldwide.[2] It is an escalating concern both in the medical and social sphere worldwide,[3] giving rise to enduring social, psychological, emotional, and mental distress, which can ultimately contribute to the emergence of various mental health conditions among couples dealing with infertility.[4]
At present, there exist multiple treatment alternatives accessible to couples grappling with infertility, such as intrauterine insemination (IUI), in vitro fertilization, and intracytoplasmic sperm injection, collectively known as assisted reproductive technology (ART).[4] These treatment methods are also widely adopted practices in neighboring countries, including Nepal and India.[4,5]
IUI is globally recommended by clinicians as the initial treatment of choice for infertile couples.[5] This preference is because, among all ARTs, IUI is considered the most cost-effective, least invasive, and preferred method.[5] Only when repeated IUI attempts fail, alternative advanced methods are typically pursued.[6]
In the past, Bhutan lacked accessible infertility treatments, which were primarily within reach for educated and affluent couples who could seek such services abroad. As the number of infertile couples in the country continued to rise, clinicians recognized the pressing need to establish infertility clinics. Consequently, in 2016, an infertility clinic was inaugurated at Jigme Dorji Wangchuck National Referral Hospital (JDWNRH). Since its inception, this clinic has provided IUI services to all infertile couples in Bhutan.
The IUI procedure necessitates semen preparation, a task performed at the clinic following the guidelines outlined in the World Health Organization manuals.[7] At the clinic, semen preparation for IUI is carried out using either the swim-up or density gradient methods, depending on the nature of the semen samples. The swim-up method is typically employed when semen samples are assessed as largely normal. In severe oligozoospermia, asthenozoospermia, or teratozoospermia, the density gradient method is usually the preferred choice for semen preparation.[7]
At the clinic, we maintained a registry to document essential information concerning couples seeking treatment. This registry contained information such as demographic characteristics, semen parameters, and the specific methods employed for semen preparation. Furthermore, we consistently document the results of pregnancy tests, indicating whether they yielded positive or negative results when female patients return for a follow-up examination approximately 14 days after the procedure.
The government made significant investments in acquiring both equipment and human resources to operate the clinic. Regrettably, as of now, no study has been conducted to assess the outcomes of IUI treatment within the country. Evaluating service outcomes holds significant importance for quality control and clinical audits within any healthcare facility, providing valuable insights for ongoing improvement and enhancement.[8]
Hence, the purpose of this study was to utilize the available data from the register and determine the outcome of IUI in the country. The findings from this study should either corroborate or challenge the government’s investment. If the findings fall short of expectations, it becomes imperative to identify the root cause of the issue so that prompt corrective actions can be implemented.
MATERIAL AND METHODS
This retrospective study was conducted through a review of the medical records of 57 infertile couples who underwent IUI at the infertility clinic of JDWNRH from January to December 2022. It is important to emphasize here that this hospital is the only facility in Bhutan that provides IUI services. As a result, couples experiencing fertility problems from different parts of the nation are referred to this hospital to avail of the IUI treatment, where processed sperm is directly inserted into a woman’s uterus to increase the chances of pregnancy.
For this study, data collection involved extracting information from the register maintained at the infertility clinic. A total of 57 couples were recorded in the register who underwent IUI between January and December 2022, covering a 1-year duration, and all of them were included in our study.
From the register, we recorded individual data points covering demographic characteristics, semen parameters, and outcomes of IUI. These records underwent a stringent double-entry process and were then subjected to comprehensive validation and analysis using IBM Statistical Package for the Social Sciences version 26.0, Armonk, NY.
A descriptive analysis was done focusing on frequency distribution. Any discrepancies or outliers within the dataset were cross-checked against the original registers to ensure their accuracy. Furthermore, we utilized the same software to calculate frequencies, percentages, and produce statistical diagrams.
Our primary outcome was the success rate of IUI, specifically in terms of achieving a positive biochemical pregnancy, rather than clinical pregnancy. A biochemical pregnancy test was done using a commercial pregnancy test kit on day 14, following IUI when the couples returned for follow-up.
Ethical clearance waiver was granted by the Institutional Review Board (IRB) of Khesar Gyalpo University of Medical Sciences of Bhutan vide Ref. No. IRB/Waiver-Exempt/PN21-0426/2021-22/519 dated February 12, 2022.
RESULTS
From January to December 2022, 57 infertile couples underwent an IUI procedure as a treatment option due to infertility problems in the country. According to age categories, a maximum 45 (78.9%) of the infertile men were within the age range of 30–39 years. For the age range of 20–29 and 40–49, there were 6 (10.5%) in each age range [Table 1]. A majority 47 (82.5%) of the infertile men had maintained a recommended sexual abstinence of 3–5 days, while 10 (17.5%) had two or fewer days of sexual abstinence [Table 1].
| Variables | Range | Frequency | Percentage |
|---|---|---|---|
| Age in years | 20–29 | 6 | 10.5 |
| 30–39 | 45 | 78.9 | |
| 40–49 | 6 | 10.5 | |
| 50–59 | 0 | 0.0 | |
| 60 or more | 0 | 0.0 | |
| Total | 57 | 100.0 | |
| Abstinence in days | 3–5 days (normal) | 47 | 82.5 |
| Two days or less | 10 | 17.5 | |
| Six days or more | 0 | 0.0 | |
| Total | 57 | 100.0 |
IUI: Intrauterine insemination
Regarding the occupation of the infertile men, a maximum of 32 (56.1%) were working in the private sector, followed by civil service 19 (33.3%). Others, including farming, private company, and armed forces, were <5% [Figure 1].
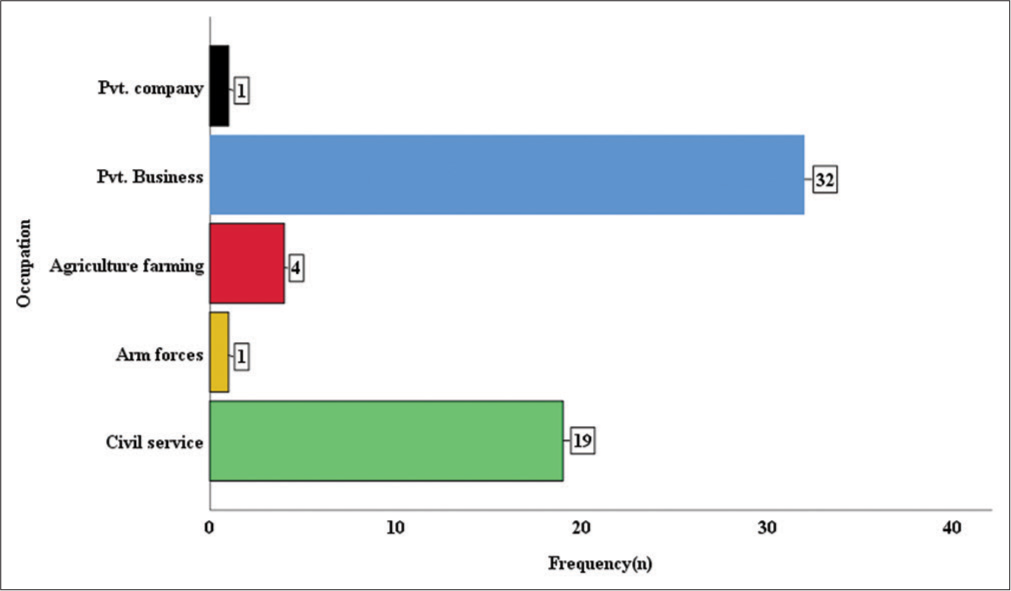
- Occupation of infertile men who underwent intrauterine insemination at the infertility clinic of the National Referral Hospital of Bhutan from January to December 2022 (n = 57).
Maximum 49 (86%) infertile men had normal semen volume between 1.3 mL and 7.6 mL per ejaculation, and only 8 (14%) had abnormal semen volume. Almost all the infertile men, 54 (94.7%), had the normal appearance of the semen, which is gray opalescent, while 2 (3.5%) had red-brown and 1 (1.8%) had a yellowish appearance. Of the included infertile men, 45 (78.9%) had a liquefaction time of <30 min, while 12 (21.1%) of them had a liquefaction time within 60 min. Almost all 55 (96.5%) of the semen were of normal viscosity, whereas only 2 (3.5%) had abnormal viscosity. A maximum of 53 (93%) of the infertile men had normal pH of the semen, which ranges between pH of 7.2 and 8, while only 4 (7%) had abnormal pH of semen [Table 2].
| Variables | Range | Frequency | Percentage |
|---|---|---|---|
| Semen volume (mL) | 1.3–7.6 mL (Normal) | 49 | 86.0 |
| Abnormal | 8 | 14.0 | |
| Total | 57 | 100.0 | |
| Appearance of semen | Gray opalescent | 54 | 94.7 |
| Red-brown | 2 | 3.5 | |
| Yellowish | 1 | 1.8 | |
| Clear and colorless | 0 | 0.0 | |
| Total | 57 | 100.0 | |
| Liquefaction time | Within 30 min | 45 | 78.9 |
| Within 60 min | 12 | 21.1 | |
| Total | 57 | 100.0 | |
| Viscosity | Normal | 55 | 96.5 |
| Abnormal | 2 | 3.5 | |
| Total | 57 | 100.0 | |
| pH | 7.2–8 | 53 | 93.0 |
| <7.2 or >8 | 4 | 7.0 | |
| Total | 57 | 100.0 |
IUI: Intrauterine insemination
Out of 57 infertile men, a maximum of 40 (70.2%) had less total sperm numbers, whereas 17 (29.8%) had normal sperm numbers. A majority of 41 (71.9%) of the infertile men had normal progressive motility, while 16 (28.1%) had less progressive motility. Around half, 34 (59.6%) of the infertile men had non-progressive motility of 20–30%, while 23 (40.4%) had progressive motility of 31–40%. More than half, 32 (56.1%), had immotile spermatozoa between 20% and 30%, whereas 25 (43.9%) had between 31% and 40% of immotile spermatozoa. Maximum 26 (45.6%) infertile men presented with oligozoospermia followed by normozoospermia 14 (24.6%) and oligoasthenozoospermia 14 (24.6%) while 3 (5.3%) presented with asthenozoospermia [Table 3].
| Variables | Range | Frequency | Percentage |
|---|---|---|---|
| Total sperm number (106/ejaculate) | Normal (≥35 million/ejaculate) | 17 | 29.8 |
| <35 million/ejaculate | 40 | 70.2 | |
| Total | 57 | 100.0 | |
| Progressive motility (%) | ≥29 | 41 | 71.9 |
| <29 | 16 | 28.1 | |
| Total | 57 | 100.0 | |
| Non-progressive motility) (%) | 20–30 | 34 | 59.6 |
| 31–40 | 23 | 40.4 | |
| Total | 57 | 100.0 | |
| Immotile spermatozoa (%) | 20–30 | 32 | 56.1 |
| 31–40 | 25 | 43.9 | |
| Total | 57 | 100.0 | |
| Diagnosis | Normozoospermia | 14 | 4.6 |
| Oligozoospermia | 26 | 45.6 | |
| Asthenozoospermia | 3 | 5.3 | |
| Oligoasthenozoospermia | 14 | 24.6 | |
| Total | 57 | 100.0 | |
| Success rate | Successful | 3 | 5.3 |
| Unsuccessful | 54 | 94.7 | |
| Total | 57 | 100.0 |
IUI: Intrauterine insemination
The outcome in terms of positive or negative biochemical pregnancy test was expressed as success rate, and the success rate of IUI in the country for 1 year was 3 (5.3%) whereas the unsuccessful rate was 54 (94.7%) [Table 3].
DISCUSSION
In the present study, we have evaluated the 1-year success rate of IUI. The findings reveal that the overall success rate of IUI in Bhutan for the period from January to December 2022 stood at a modest 5.3%. It is noteworthy that this success rate is considerably lower compared to the rates observed in neighboring countries and various western nations. The success rate of IUI varied across different countries, with
Nepal reporting a rate of 15.7%,[5] India ranging between 10% and 20%,[9] Sri Lanka at 15%,[10] Pakistan between 16% and 20%, and the USA achieving 20% success.[11,12] These variations in success rate can be attributed to a multitude of factors. Key determinants include the age of the couples, semen quality, precise timing and frequency of IUI procedure, availability of advanced laboratory facilities, as well as the expertise, knowledge, and training received by the healthcare staff.[11,13,14] Likewise, the plausible factors that might influence the IUI success rate in our study could be attributed to acute shortage of staff, lack of reskilling and upskilling for the staff, and absence of standardized facilities and equipment at the clinic. These factors may account for the observed low IUI success rate in the country. The most concerning aspect of our findings is that 54 out of 57 couples (94.7%) who underwent IUI experienced unsuccessful outcomes. This high rate of failure is deeply troubling. Among these infertile couples, many did not have access to alternative treatment options within the country. A few who could afford it sought treatment abroad at their expense, but the majority were left without viable options locally as they could not afford the treatment abroad. As awareness of alternative options in other countries grows, combined with the rising trend of delayed childbearing and increasing insurance coverage, it is anticipated that there will be a surge in the number of couples seeking infertility treatment. Consequently, it is crucial for the Ministry of Health to proactively plan and act to introduce newer and more advanced alternative treatment options within the country.
In this study, the majority of the infertile men were in the age range of 30–39 years, which is consistent with the observations in numerous other studies.[5,15-17] Male age has a significant effect on pregnancy outcomes owing to its impact on sperm quality. Research has revealed that as male subjects grow older, there is a decrease in sperm volume, concentration, and vitality, which can be correlated with infertility.[6] The physiologic consequences of advancing age on the male reproductive system are an identified factor contributing to infertility.[6] However, it is worth noting that our study does not delve into the specific effects of age on fertility, indicating a need for further investigation in this regard.
In our research, a significant proportion of men exhibited below-average total sperm counts, and the majority also displayed high percentages of non-progressive and immotile spermatozoa. The most common semen abnormalities in our study were oligozoospermia, followed by oligoasthenozoospermia and asthenozoospermia. These findings might have affected the outcome of IUI in the country. These factors were also identified by several studies as contributing factors to infertility.[9,18,19]
The major strength of our study is the comprehensive nature of our study population. As the only clinic in the country offering both semen analysis and treatment services, the sample utilized in our study closely resembled a representative cross-section of the entire national population, allowing for the generalizability of our findings to the entire country. Furthermore, this pioneering study stands as the first of its kind to date, producing invaluable and evidence-based scientific data regarding the outcomes of IUI within the country. These findings hold substantial significance for future references, informing policy planning at all administrative levels, resource allocations, the prioritization of human resource investments, and training and knowledge enhancement. Ultimately, this data has the potential to enhance the success rate of IUI procedures within the nation. Conversely, this study has some limitations, too. The first one was the clinic’s limited infrastructure, human resources, and expertise. The other limitation was the retrospective nature of our study. Our analysis relied solely on pre-existing data within the clinic’s records, potentially introducing a bias based on the information available, and therefore, the results may not be directly extrapolated to other findings.
CONCLUSION
Considering the comparatively lower success rate of IUI in our country when compared to neighboring nations, there is an imperative need for a resolute commitment and the implementation of robust strategies. This effort is essential to elevate our success rate to align with international standards and effectively address the growing challenge of rising infertility rates within our population. Furthermore, a deeper understanding of the factors that underlie the country’s suboptimal IUI success rate is paramount. The insights gleaned from additional scientific studies can inform strategic revisions in planning and policy-making, offering a ray of hope to couples grappling with infertility issues.
Acknowledgments
The authors would like to express their gratitude to all the participants for allowing the use of their records in the study.
Ethical approval
The research/study was approved by the Institutional Review Board of KGUMSB, vide Ref. No. IRB/Waiver-Exempt/PN21-0426/2021-22/519 dated February 12, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Fertility and infertility: Definition and epidemiology. Clin Biochem. 2018;62:2-10.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of infertility in couples. J Nepal Health Res Counc. 2019;17:85-9.
- [CrossRef] [Google Scholar]
- Selected risk factors and pattern of semen abnormality in male partners of infertile couples in Eastern Nepal: A descriptive cross-sectional study. J Nepal Med Assoc. 2020;58:668-71.
- [CrossRef] [PubMed] [Google Scholar]
- Role of mental health practitioner in infertility clinics: A review on past, present and future directions. J Hum Reprod Sci. 2018;11:219-28.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of intra uterine insemination in Sahara international fertility centre Pokhara, Nepal. Med J Pokhara Acad Health Sci. 2018;1:105-9.
- [CrossRef] [Google Scholar]
- The effect of female age on the outcome of intrauterine insemination treatment in a public hospital-assisted reproduction technology unit. Niger J Clin Pract. 2018;21:988-92.
- [CrossRef] [PubMed] [Google Scholar]
- WHO laboratory manual for the examination and processing of human semen. . 2021;5:286. Available from: https://whqlibdoc.who.int/publications/2010/9789241547789_eng.pdf [Last accessed on 2023 Oct 25]
- [Google Scholar]
- Quality control application in healthcare management. Trauma Acute Care. 2017;2:30.
- [Google Scholar]
- Intra uterine insemination treatment. 2022. Available from: https://fertilityclinicmumbai.com/treatments/iui-intra-uterine-insemination [Last accessed on 2023 Oct 25]
- [Google Scholar]
- The effect of atmospheric temperature on the outcome of intrauterine insemination. Pak J Med Sci. 2008;24:127-9.
- [Google Scholar]
- Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99:1324-31.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting success of intrauterine insemination: A 3-year prospective study. Int J Reprod Contracept Obstet Gynecol. 2016;1:1077-83.
- [CrossRef] [Google Scholar]
- Factors influencing the success rate of intrauterine insemination: A retrospective study in Sultan Qaboos university hospital. J Womens Health Care. 2017;6:402.
- [CrossRef] [Google Scholar]
- The effect of age, ethnicity, and level of education on fertility awareness and duration of infertility. J Obstet Gynaecol Can. 2014;36:990-6.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, perceptions and myths regarding infertility among selected adult population in Pakistan: A cross-sectional study. BMC Public Health. 2011;11:760.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of male factor and abnormalities of semen analysis in infertile couple. Prof Med J. 2020;27:1454-8.
- [CrossRef] [Google Scholar]
- Prevalence of infertility in a cross section of Pakistani population. Pak J Zool. 2010;42:389-93.
- [Google Scholar]
- Impact of age on semen parameters in male partners of infertile couples in a rural tertiary care center of central India: A cross-sectional study. Int J Reprod Biomed. 2017;15:497-502.
- [CrossRef] [PubMed] [Google Scholar]