Translate this page into:
Menstrual cyclicity: Pathogenicity, predictability, and reproducibility

*Corresponding author: Amlan Kanti Ray, Department of Reproductive and Cancer Genetics, Diverse Genomics Private Limited, Kolkata, West Bengal, India. humanedestiny@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ray AK, Roychoudhury M. Menstrual cyclicity: Pathogenicity, predictability, and reproducibility. J Reprod Healthc Med. 2024;5:16. doi: 10.25259/JRHM_15_2023
Abstract
The birth of every female child triggers the potential risk of endometriosis is yet to be ascertained. It has brought about the understanding of the untraceable pathophysiological relation between endometriosis and the onset of the menstrual period. It is an estrogen-dependent benign inflammatory disease characterized by the presence of ectopic endometrial implants such as endometrial glands and stroma outside the uterus. The occurrence of the earlier menarche before the onset of the adolescent stage is no longer restricted to the exposure of such metabolic disease. Rather, it is further extended to the normative and the late menarche according to the evidence-based studies. The widespread pathophysiological developments in different menarcheal age and its impact is implicated in disease onset has spurred researchers to investigate a causal relation between the range of menarcheal age and the concomitant increase of civilization chronic diseases due to having multiple factors which directly exacerbate a high degree of the metabolic investment in the widest area of the reproductive functioning, menarcheal age, nutritional status, and parity by virtue of the inextricably interwoven of complexity between the menstrual cycle and pathogen load of the retrograde menstruation. An evolutionary menstrual cyclical model predictably modulates hormonal milieu, inflammation, estrogen exposure, and pinpointing the migration of endometrial debris into the peritoneal cavity, which is up-regulated in the menstrual cycle and eventually increases the chances of the development of estrogen-dependent disease such as endometriosis. The present review evaluates the published evidence on the potential risk of endometriosis irrespective of any menarcheal age.
Keywords
Menarche
Menstrual cyclicity
Menstruation
Mean age
Endometriosis
INTRODUCTION
Menarche marks the range of the reproducibility age of Homo sapiens with the beginning of the menstrual cycle in a woman’s reproductive career. It is likely to be linked to acquiring the aid needed for successful reproductive outcomes.[1] Its proximate cause is an increase in the frequency of the gonadotropin-releasing hormone (GnRH) pulse generator in the hypothalamus.[2,3] Pubertal events due to the activation of the hypothalamic-pituitary-gonadal (HPG) axis and hypothalamic-pituitary-adrenal axis cluster together and follow a fairly uniform sequence, whose end program is menarche, conform to a biological and timing of maturation.[4] The HPG axis regulates neuroendocrine function to facilitate the release of GnRH, leading to a rise in pulsatile secretion of gonadotropins such as, follicle-stimulating hormone and luteinizing hormone from the anterior pituitary, activating the onset of ovulatory menstrual cycles.[5] The ovary’s estrogen and progesterone influence the uterus’s control of each other’s actions through a complex set of negative feedback loops.[6] Women’s experience of menarche and menstruation is a complex interweaving of their particular physiology,[7] psychology,[8] and cultural backgrounds.[9] A paradigm shift from childhood to womanhood has been subject to extraordinary symbolic elaboration in various cultures. Such representative strength is so frequently ascribed to feminine blood, and the colorful appearance of rules for the direction of discharging ladies has put the monthly cycle in closer view of the anthropological investigations of “taboo”[10,11] and “contamination.”[12,13] Concentrating reports in the UK and the USA uncovered that ladies would not talk about their period to anyone. Study reports in the UK and the USA reveal that women would not discuss menstruation with all people.[14] Laws[14] called it “menstrual etiquette,” which describes certain boundaries around women’s menstrual behavior.[14] Understanding the concept of “menstrual etiquette” and its impact on women’s health is crucial for understanding the social and cultural factors that can affect women’s reproductive health.
The widespread occurrence of different menarcheal ages[15] and their impact on disease onset have spurred researchers to investigate a causal relationship between the downward secular trend[16] of menarcheal age and the concomitant increase of civilization’s chronic diseases.[17] Several factors[18] have been shown to significantly influence the age at menarche, such as programmed patterns of gonadotropin release established during antenatal ontogenesis, genetic parameters,[19] socioeconomic conditions,[20] general health and lifestyle,[21] nutritional status,[22] seasonality,[23] physical activity,[24] and altitude level.[25,26]
MENARCHE AND RISK OF ENDOMETRIOSIS
Menstruation is the monthly shedding of the endometrium, which occurs naturally during the reproductive age of women. This could be explained by the cyclicity of the endometrial shedding[27] and the vaginal bleeding.[27,28] During each cycle, endometrium proliferates, developing a higher secretory capability followed by an extended microvasculature. If implantation and pregnancy do not occur, the extra tissue is reabsorbed or shed with the menses.[27] Vaginal bleeding,[27,28] on the other hand, is the external loss of blood and other tissues through the vagina. The capability of endometrial cycles is that they are coupled to ovarian cycles. Regular menstruation is a marker of sterility, not fecundity. The fecund women mostly conceive on one of their postpartum cycles, whereas the less fecund women continue to cycle regularly.[29]
Menstrual cyclicity is a set of routine patterns that conform to the average length (21–35 days)[30] of the monthly cycle regulation of four subsequent phases: Follicular phase, ovulatory phase, luteal phase, and menstrual phase. Phasal changes are regulated by the internal production of hormones from the pituitary gland. Thus, due to having an intricacy in the central nervous system involving the ovaries and the uterus, an exposure to menstrual periods occur.[30] Alteration of any phase due to hormonal imbalance or immunological disorder results in changes in cyclicity and is implicated in reproductive disease. Menstrual cyclicity and prostaglandin-inflammatory dynamics play a plausible role (prostaglandin metabolism, and immunological factors have been suggested) to cause endometriosis potentially. Possible reasons of incessant menstruation are (the factors most consistently associated with) early-age onset with often occurrence of high and low flow during (menarche and long and heavy menstrual cycles reflect increased exposure to reproductive complications) menstruation.[31] Early menarche is associated with a more rapid onset of ovulatory cycles and the tendency to sustain higher levels of progesterone and estrogen in secretory phase (of luteal phase estradiol and progesterone).[32,33] Menarche exemplifies the foci of differential menstrual cyclicities as symptoms linked with a possible reproductive disorder such as endometriosis.
Onset of menses begin (menarche typically occurs) within the age range of 9–16 in girls, although the age varies across and within different groups of populations. Widely published literature on early maturation, faces an array of disagreement (having a substantial controversy) pertinent to the upper and lower limit of (over age cutoffs for determining) early menarcheal age. The wide range of early menarche [Table 1] is implicated in early biological maturity. There is a lower limit of ≤8 years[34] and an upper limit of <12 years[35] in the category of early menarche. Understanding this age range is crucial, as it can help identify potential health risks and implications for early or late menarche.
| Country | Study Population | Design | Cases | Controls | Parameter | Results | Remarks | Source |
|---|---|---|---|---|---|---|---|---|
| Australia | Women are recruited from a genetic study of endometriosis and the Australian Twin Registry between 18 and 55 years of age | Case-control | 268 women with laparoscopically confirmed endometriosis | 244 women matched to age and geographic location are recruited from the Australian Twin Registry | Mean & SD menarchial age for cases and controls | Endometriosis among women <12 years at menarche (SD ..4 y) (OR= 1.3; 95% CI, 0.5- 3.4) compared with those ≥14 years at menarche 0.3; 95% CI, 0.1-0.6 | Women with endometriosis are less in late (≤14 years) compared to early menarche (OR= 0.3;95% CI, 0.1– 0.6) | Treloar et al.,2010[40] |
| Belgium | Women attending gynecology clinics with the mean age of 32.9 (SD.5.5y) in Deep endometriotic nodules (DEN) group and 33 (SD. 6.1 y) in Peritoneal Endometriosis (PE) group | Case-control | 88 prospectively enrolled cases of laparoscopically diagnosed endometriosis | 88 age-matched hospital controls without complaints of infertility, pelvic pain, or dysmenorrhea | Median & range of age at menarche for cases compared with controls | Endometriosis among women 12.5(OR= 0.86; 95% CI 0.68- 1.10) in DEN and 13 (OR= 1.0; 95% CI 0.84- 1.28) | Menarchial age under 12.5(OR= 0.86; 95% CI, 0.68-1.10) in DEN and 13 (OR= 1.0; 95% CI, 0.84-1.28) in PE groups evidently shows the risk of endometriosis | Heilier et al., 2007[42] |
| Canada | Women recruited from 10 clinical institutions in and around Montreal between <30 and >40 years of age | Case–control | 896 women retrospectively enrolled with surgically confirmed endometriosis | 1881women having age- matched controls with no surgical evidence of the disease | Odds of endometriosis in women ≤11 years at menarche compared with those >11years at menarche | Odds of endometriosis remained significantly different in both subgroups (OR=1.6; 95% CI, 1.2 -2.2) for hysterectomy (OR= 1.5; 95% CI,1.2- 2.2) | No association of (≤11 - >11) found in three surgical categories | Hemmings et al., 2004[43] |
| Canada | Women aged 20- 39 years, infertile undergoing diagnostic laparoscopy | Case-control | 329 prospectively enrolled cases with laparoscopically diagnosed endometriosis | 262 controls were women (from same cohort) who did not have endometriosis | Odds of endometriosis in women ≤13 years at menarche compared with those ≥14years at menarche | 13 years (POR= 1.63 ;(95% CI, 1.02-2.60) & ≥14 (POR = 1. 73;(95% CI 1.07- 2.78) | Odds of rASRM stages I or II endometriosis increases among women of 13 years | Bérubé et al., 1998[44] |
| Canada | Women of less than 42-years- old after histologically confirmed endometriosis | Case-Control | 789 women prospectively enrolled after laparoscopically diagnosis of endometriosis | 576 women controls (from same cohort) | Mean & SD of age at 13.0 (SD. 1.7 y (SUP*); 12.9 (SD.1.5 y (OMA*); & 12.9 (SD.1.5 y (DIE*) *SUP: superficial endometriosis, *OMA: endometrioma, *DIE: deep infiltrating endometriosis | <12 years under SUP (OR= 1.2; 95% CI, 0.8–1.9); OMA (OR= 0.9; 95% CI, 0.6-1.4) DIE (OR= 0.9;95% CI, 0.6-1.4) >13 years under SUP (OR= 1.3; 95% CI, 0.9-1.8); OMA (OR= 0.9; 95% CI, 0.6 –1.2) DIE (OR= 0.9; 95% CI, 0.6–1.2) | Early menarche (<12 years) and late menarche (>13 years) were not associated with the endometriosis phenotype (ns) | Marcellin et al., 2019[45] |
| Egypt | Women enrolled from the University Hospital,, Alexandria aged 16 - 43 years | Case-control | 110 women diagnosed with endometriosis | 220 women hospital-based, age-matched controls. | Odds of endometriosis in women ≤11 years compared with those 12 years at menarche | ≤11 years (OR=2.2; 95% CI, 1.19-4.22) &12 years (OR=1.2; 95% CI, 0.65–1.91) | Plausibility of endometriosis is found in early ≤11 years, (P<0.05) menarche versus controls | Mamdouh et al., 2011[36] |
| France | Prospective E3N cohort of French women aged 40- 65 are enrolled | Nested case- control | 2684 women are surgically ascertained with endometriosis | 75,918 women as controls | Endometriosis risk was first assessed in models adjusted for age at menarche (<12, 12-14 , ≥15 years | <12 years (AOR= 1.19; 95% CI, 1.09- 1.31) & ≥ 15 years (AOR= 0.90; (95% CI, 0.78-1 .04) P < 0.0001 | Earlier menarcheal age of <12 years and shorter menstrual cycle length were associated with a higher risk of endometriosis. Or endometriosis alters the hormonal milieu, disrupts cyclicity | Kvaskoff et al., 2013[46] |
| Germany | A pool of 595women as cases and 475 women as controls enrolled in a hospital- based Bavarian Endometriosis Study | Case–control | Age-matched laparoscopically confirmed 298 cases | 300 women as controls after matching for age | Odds of endometriosis in women ≤11 years compared with those ≥15 years | ≥15 years (OR=0.44; 95% CI, 0.23 - 0.87) compared to ≤11 | Menstrual characteristics other than age at menarche are evaluated as predictive marker for endometriosis | Burghaus et al., 2011[47] |
| India | Women in the age group between <29 & ≥40 years recruited from Assam Medical College & Hospital Dibrugarh | Observational | 89 women recruited after laparoscopically diagnosed of endometriosis | Mean & SD of age at menarche for cases | mean 11.45 years (SD.1.24 y) | Trend of increasing risk of endometriosis at mean age at 11.45 years | Udupa et al 2023[62] | |
| Iran | Women recruited aged 20 - 50 with or without endometriosis from Alzahra Hospital | Case-control | 185 women of reproductive age with confirmed endometriosis | 370 women of reproductive age without endometriosis admitted for other issues | Odds of endometriosis in women ≤12 years compared with those >12 years | Risk of endometriosis is 5-times higher in one sub- group (OR=5.3; 95% CI, 2.16 - 12. 66), 3-times higher in another sub- group (OR=2.90; 95% CI, 1.28 - 6.55) in the age at menarche of 12 years | Risk of endometriosis has not been related with the age of menarche | Mollazadeh et al., 2019[48] |
| Italy | Infertile women aged 23–44 years, scheduled for laparoscopy | Case-control | 50 prospectively enrolled cases; infertile women with laparoscopically diagnosed endometriosis | 47 infertile women (from same cohort) without endometriosis infertile women | Odds of endometriosis in women ≤11 years compared with those ≥13 years | OR=1.4; 95% CI, 0.5-4.6 (fertile control) OR=2.2; 95% CI, 0.5-9.2 (infertile control) | Weak association (fertile controls) between age at menarche of ≤11 (OR=1.4; 95% CI, 0.5-4.6) compared to stronger association (infertilecontrols) of ≤11 (OR=2.2; 95%CI, 0.5-9.2) withendometriosis | Signorello et al., 1997[39] |
| Italy | Women aged 20-49 attending different hospitals in Lombardy | Case-control | 376 prospectively enrolled cases with infertility, pelvic pain, or pelvic masses after laparoscopically diagnosed endometriosis | 522 hospital controls with acute conditions attending hospitals | Odds of endometriosis in women ≤11years compared with those ≥14 years | Risk is found in menstrual characteristics other than age at menarche (OR=0.3; 95% CI, 0.2 - 0.7, <0.05) (rASRM of stage I), (OR=0.5; 95% CI, 0.2 - 1.2) (rASRM of stage II), (OR=0.5; 95% CI, 0.2 - 1.0, <0.05) (rASRM of stage III) and ), (OR=0.3; 95% CI, 0.1- 0.9, <0.05) (rASRM of stage IV) | Early menarche seems to be a risk factor but remains unclear | Parazzini et al., 1995[49] |
| Italy | Women aged 24-48 admitted to the hospital of the University of Milan, and the Clinic of Brescia and Pavia, Lombardy, Northern Italy | Case-control | 241 prospectively enrolled cases with infertility, pelvic pain, or pelvic masses, and laparoscopically diagnosed endometriosis | 437 hospital controls with acute conditions, attending hospitals | Odds of endometriosis in women ≤11 compared with those ≥14 years | Plausibility of lower risk is found in menstrual characteristics other than age at menarche (RR= 0.3; 95% CI, 0.2 - 0.5) . | Relative to women, whose menarche occurred at age 11 or younger, the risk of endometriosis was slightly lower in those who experienced later menarche, but the trend in risk wasnot significant | Candiani et al., 1991[50] |
| Malaysia | Women aged 19-45 admitted to University Hospital in Kuala Lumpur and the General Hospital in Johore Baru | Case-control | 305 prospectively enrolled women with laparoscopically diagnosed endometriosis | 305 age-matched hos- pital controls with fibroids, ovarian tumours, EP, DUB, pelvic inflammatory disease, and infertility | Odds of endometriosis in women <12 years compared with those ≥12 years | OR 0.86 (95% CI 0.42–1.45) | Age at menarche < 12 years other than menstrual characteristics is not significantly associated with endometriosis | Arumugam and Lim K, 1997[51] |
| Nigeria | Women recruited from Lagos, Nigeria | Case-control | 113 women retrospectively collected from the medical records with endometriosis | 113 women control from same cohort without endometriosis | Odds of endometriosis in women <11 years compared with those 11- 13.9 & ≥14 years | <11 years (OR= 1.80; (95% CI, 0.51- 6.33); 11 – 13.9 years (OR= 1.61; (95% CI, 0.94- 2. 74)≥ 14.0 years (OR= 0.54; (95% CI, 0.31- 0.94) | The plausibility of endometriosis much higher (OR=1.80; 95% CI, 0.51- 6.33) age at age <11 compared to 11.13.9 years(OR=1.61; 95%CI,0.94- 2.74).Correspondingly becomes very low (OR=0.54; 95% CI,0.31- 0.94) at ≥14years | Ajayi et al., 2021[52] |
| Spain | Infertile women scheduled for laparoscopy in the Hospital of Cruces, Baracaldo (Vizcaya), Spain | Case-control | 174 prospectively enrolled cases with laparoscopically diagnosed endometriosis | 174 controls (from same cohort) who did not have endometriosis on laparoscopy | Odds of endometriosis in women ≤12 years compared with those >12 years | OR 1.2,95% CI 0.8–2.0) | Earlier age at menarche seems to be a risk for developing endometriosis | Matorras et al., 1995[53] |
| Sweden | Women included a cohort of 28,822 female twins aged 20–65 with mean age 44.45 (SD.12.30) participated in two cross sectional surveys of Swedish Twin Registry | Case–control | 1,228 women were recruited after laparoscopically diagnosed with endometriosis | 26,527 women are included in the study as controls | Odds of endometriosis in women <11 years compared with those 15 years | Age at menarche 14 years (OR=0.75; 95% CI, 0.60- 0.93) and age at menarche 15 years (OR=0. 63; 95% CI, 0.60-0.93). | An inverse association between late menarche and risk of endometriosis | Saha et al., 2017[54] |
| UK | Women recruited for lap-sterilization, chronic pelvic pain & abdominal hysterectomy for DUB | Case-Cohort | 201women prospectively recruited after laparoscopically diagnosed endometriosis | 721 controls (from same cohort) who did not have endometriosis after laparoscopy | Mean & SD of age at menarche for cases and cohort | Cases: mean 12.84 years (SD 1.53 y); controls: mean 13.23 years (SD 1.50) | Relationship between the age at menarche and endometriosis is not assessed | Mahmood et al., 1991[61] |
| USA | women aged 18-44 enrolled in operative cohort in comparison with an age- and residence- matched population cohort unexposed to population cohort | Cohort | 495 cases under operative cohort | 131controls under population cohort | Odds of endometriosis in women ≤11 years compared with those ≥14 years | OR=1.05; 95 % CI, (0.94-1.17) OR=1.25;95% CI, (0.84–1.85) | Age at menarche is found no association with endometriosis | Peterson et al., 2013[59] |
| USA | Anonymous questionnaire was given to 1285 Puerto Rican women | Cohort | 57 women of self- reported cases of endometriosis | 1228 controls | Mean and SD of age at menarche for cases and cohort | No associations of endometriosis is found with age at menarche | Flores et al., 2008[34] | |
| USA | Women traced from California state hospital patient discharge records having no prior history of endometriosis | Cohort | 229 women recruited from a surgical diagnosis of endometriosis | 43,493 women are age-matched and taken as control of disease-free | Odds of endometriosis in women ≤10 years compared with those ≥15 years | ≤10 years (POR= 0.52 ;(95% CI, 0.26- 1.05); 11years (POR=1.08;95%CI, (0.74-1.59) 12 years (POR=0.83;95% CI, 0.59- 1.16); 13 years (POR=1.0);14 years(POR=1.00;95% CI,0.65-1.53); ≥15 years(POR=0.78;95% CI,0.44-1.36) | Hardly had any consistent pattern of endometriosis risk with age at menarche | Templeman et al., 2008[60] |
| USA | A retrospective review in the Division of Reproductive Endocrinology and Infertility at Yale University, USA of women with laparoscopy diagnosed pelvic endometriosis | Case-control | 535 retrospectively enrolled women using rASRM score with pelvic pain and infertility and laparoscopically diagnosed endometriosis | 200 women as control group with tubal infertility without endometriosis through surgical confirmation | Mean & SD of age at menarche for cases and cohort | Cases: mean 12.3 years (SD 1.4 (9-18 y); controls: mean 12.8 years (SD 1.4 (9-17 y) | Increased risk for endometriosis in early menarche X2 = 5.08; P < 0.024) | Matalliotakis et al., 2008[55] |
| USA | 84 women aged 18-40 undergoing laparoscopy was enrolled | Case-control | 32 women prospectively enrolled from the laparoscopy cohort | 52 women as controls without any endometriosis | Mean & SD of age at menarche for cases and cohort | ≤11years (OR= 0.2; 95% CI, 0.03–0.7); ≥14 years (OR=1.3; 95% CI, 0.5–4.0) | Age at menarche with the risk of endometriosis is not evaluated | Buck Louis et al., 2007[56] |
| USA | Women are collected in the Nurses’ Health Study II cohort from 25 to 42 years and residing in one of 14 states in the United States | Cohort | 1,721 women of laparoscopically confirmed endometriosis are enrolled | 726,205 women are recruited as controls | Mean & SD of age at menarche for cases and cohort | <10 to 12 years (95% CI, 1.0 -1.8) (<.001) | Risk of Endometriosis increases with earlier age at menarche | Missmer et al., 2004[38] |
| USA | Women aged 19- 45 recruited from a gynecologic speciality clinic in western New York | Case-control | 104 women prospectively selected with laparoscopically diagnosed endometriosis | 100 women as controls with condition other than endometriosis | Odds of endometriosis inwomen <12 years compared with those ≥12 years | Cases: mean 12. 4 years (SD 1.3 y); controls: mean 12.7 years (SD 1.6 y) pertinent to <12 years (AOR=10; 95% CI, 04-2.7) and ≥12 years (AOR=1.0) | Risk of Endometriosis with the increasing exposure to menstruation is inconclusive | Darrow et al., 1993[57] |
| USA | This is a multicenter study | Case-control | 268 women with primary infertility after laparoscopically diagnosis before prospectively enrolled | 3,794 women admitted for delivery at seven collaboratinghospitals | Odds of endometriosis in women ≤11 years compared with those ≥16 years | Cases: mean 12.4 (SD.0.08 y) Controls: mean 12.7 (SD.0.01y); ≤11 years (RR=1.2; 95% CI, 0.9-1.7) (ns); ≥16 (RR=0.8; 95& CI, 0.4, 1.7) (ns) | A trend for women with endometriosis in early menarche is not documented | Cramer et al., 1986[58] |
SD: Standard deviation,CI: Confidence interval, OR: Odds ratio, rASRM: Revised American society for reproductive medicine, SUP: Superficial endometriosis, OMA: Endometrioma, DIE: Deep infiltrating endometriosis, POR: Prevalence odds ratio, ns: Not significant, RR: Relative risk.
It is now readily apparent about consistent age pattern related to the menarche, which varies from ≤8 to <12 years. The consistent controversy surrounding the early age category of menarche may attenuate a reasonable growing potential bias [Table 1] arising from the different studies, either through a universal consensus or by maintaining a strict methodology of clearly mentioning the category to be followed by investigators through cutoff marks. The differential age in the early menarche category is likely to impede the analysis that demands further investigation exploring or analyzing infertile and adolescent populations taking different pathological details of the disease (with endometriosis separately). An early manifestation of maturation occurring at <12 years of age has a possibility of facing reproductive anomaly leading to (associated with a higher risk of) certain health issues, including estrogen-driven disease envisages (endometriosis, and other anomalies) that this concept is crucial for identifying potential health risks associated with early puberty.
The mean onset of period becomes the most important indicator pertinent to the women’s sexual maturity due to the reliability for diagnosis.[36] Mean onset (average age of menarche) declined from about 17 to 12.8 from 1830 to 1962. The cessation of the drift (trend has stopped) occurs simultaneously with the concomitant progress of cyclicity influences the leveling off at 12.6.[37]
The majority of the hitherto epidemiologic researches on endometriosis[38] is centred on menstrual cyclicity[39] along with allied pathological conditions.[40] Due to the exposure to menstruation in the entirety of procreative age, all putative menstrual factors could be the plausible exposure to (risk of developing) endometriosis.[41]
Among 26 studies [Table 1] evaluated from the review of literature, 20 are case-control, one is case-cohort, four are cohort, and one is an observational are accessible on-line have been retrieved from the year 1986 to 2023. Twenty reports collectively demonstrate (case-control studies involving) 9073 diagnosed women as cases versus (cases of laparoscopically diagnosed endometriosis) 4,12,130 controls,[36,39,40,42-58] four cohorts have 201 cases and 7,71,157 controls,[34,38,59,60] one each case-cohort (201 cases vs. 721 controls),[61] and observational study with 89 cases, respectively, were conducted [Table 1]. The case-control studies were conducted in three in the USA, three in Canada, three in Italy, and rest ten studies were executed in Oceania, central European countries (conducted in Austria, Belgium), Egypt, France, Germany, Iran, Malaysia, Nigeria, Spain, and Sweden. One each case-cohort and observational research had been aimed at UK and India, respectively, and rest four cohort projects had been selected from USA. Study population was predominantly from general (representative of source) population. Above reports belonged to either used population control other than hospital[34,40,43,47,55-57,59] of subjects that are were derived from the same group (sampled from the same cohort)[39,44,45,52,53,61] or from hospitals.[37,41,47-49,62,63] However, four studies[38,46,54,60] had been sampled from controls from large population cohort.
Women under study are by and large under 18–>50 years of age, although two of them were recruited to the tune of 65 years.[46,54] Among them, five studies[39,44,53,55,58] belonged to sub-fertile, although a single study comprised of infertile women was case–control studies was mentioned on (the impact of) sexual activity for developing excess estrogen exposure among different subgroups are pertinent to the beginning of periods arguably from the age group of 12 onwards.[48] All but 15 studies[36,39,40,42,44-47,49-51,53,56-58] recruited women over time before (prospectively enrolled women with) laparoscopic diagnosed endometriosis. There are altogether three studies[38,43,52] which were retrospectively designed. Twenty-one studies were designed taking women experienced exposure to menstruation in advance, which are conducive to (early age at menarche as) variability in six categories such as ≤10 for (years old in) one study;[56] as <10 in one study;[38] <12 in six studies;[40,45,46,51,57,62] ≤12 in two studies;[48,53] ≤11 in nine studies;[36,39,43,47,49,50,56,58,59] and <11 in two studies.[52,54]
Seven of the 26 studies depicted a positive association with early menarche.[38,39,46,55] Two studies found less exposure to disease in the advancement of (reduced risk of endometriosis with early) menarche.[49,50] Four studies suggest a statistically significant positive trend of disease (risk of endometriosis with early menarche)[36,39,46,55] and followed by a negative trend (lesser risk in one study) when associated with fertile controls.[39,49] Two studies pooled data belong to (enrolled women with) the revised American society for reproductive medicine (rASRM) stages I or II.[44] One study from (recruited women with) rASRM stages III or IV,[49] one study with endometriosis phenotypes[64] such as superficial endometriosis (SUP), endometrioma (OMA), and deep infiltrating endometriosis (DIE)[45] were conducted. It is a sensitive indicator for public health trend analysis, clinical application, geographical location, environmental condition, and a deeper understanding of the socioeconomic inequalities within the country’s population.[65,66] While describing women living on either side of the equator (a geographic north-south gradient in age at menarche), it reveals[67] that women beyond the tropic of cancer exposed to advanced onset of period in comparison to the women who live on (girls who live at higher latitudes appear to have an earlier initiation of menses than girls who live closer to the) equator.[68] Researchers from the The National Health and Nutrition Examination Survey (NHANES) use menarcheal data from the U.S. population to understand pubertal trends in varying populations of girls.[65] The average age at menarche provides an index of variability in puberty timing and is considered the baseline of demographic variables.[69] The global-level health facilitates women in the middle-and-low-income countries to avail (and development community would greatly benefit from the increased availability of) qualitative information regarding the comprehensive details of menstrual kinetics and its respective impact on the social dynamics across the globe (data on the average age of menarche facilitates to track trends in socioeconomic and nutritional status in regions around the world).[65] Although, the improved living and environmental conditions following birth presumably strengthen the early maturation process, they too become held responsible for (or being associated with) many adverse health outcomes.[70] The evidence-based findings worldwide seem plausible and are in agreement with the evidence on (consistent with the hypothesis that) the early age of menarche that is influenced by programmed patterns of gonadotropin release formed during antenatal ontogenesis.[17] Hence, seemingly impact on such causal relation between early menarche and a woman’s reproductive career[71] is likely to being susceptible to chronic diseases later in life.[17] The phenomena of acceleration of pubertal onset in girls followed by advanced maturation could reasonably support the concerned hypothesis of Developmental Origin of Health and Diseases (DOHaD). [72] According to the DOHaD that the advanced onset has been implicated in critical windows of human individual development, which are peri-conceptional context, pertinent to fetal periods, childhood, and until the period of puberty[73,74] are by and large supposed to be the sensitive to epigenetic changes for programming human development having a probable impact on (in the risk of) chronic diseases in adulthood. This explains the worldwide downward secular trend[75] in differential onsets of periods vis-à-vis (of age at menarche) on the concomitant rise of estrogen-dependent metabolic diseases,[31] for instance, estrogenic exposure (such as endometriosis), and breast cancer.[4]
Emerging evidence suggests that the menarche is the starting point of executing (the evolution of) the spontaneous decidualization process (the “preparation,” i.e., the endometrial part for gestational development [of the endometrium for pregnancy)],[76] including the monthly the menstrual cycle has far-reaching implications for pathogenic causes of diseases. Shedding of endometrium causes pathogen load to be tightly connected, courtesy of retrograde menstruation.[77] Every female is born with the potential pathogens load of fibroids and endometriosis, whose trigger is still not being fully identified.[78] We argue that enough credible evidence exists to substantiate the hypotheses that early, normal, and late menarche have an asymptomatic relationship either between an advanced or late onset of endometriosis.
MENARCHE: THE GATEWAY OF ENDOMETRIOSIS?
Considering restrictions on knowledge of estrogen-caused disorders with underlying pelvic anomalies; requirements of further evidence-based research are a matter of urgency to expedite the cause and effect between menstrual cyclicity and progression of estrogenic responses in the ectopic milieu (having a greater limitation to our current understanding of how endometriosis develops, challenges to reproductive health are being elucidated by several studies highlighting the different reproductive patterns and the associated hormonal cycles). Reflections from population studies state that endometriosis is lately diagnosed, because the onset of the disease is hidden under the guise of “menstrual etiquette.” However, it quietly alternates menstrual cyclicity to be developmentally entrained contingent on pathological risks using draining out the menstrual reflux into an ectopic region (the peritoneal cavity) which may likely to form endometriotic implants either in the early menarche; in the normative menarche; in subsequent phase of (in the late) menarche or where, menarcheal age is not in the etiological route to cause sequence of reactions on the surface of the ectopic region.
Early menarche
Early menarche causes early onset of ovulation and regular menstrual cycle.[41] Increasing exposure to generating retrograde factors[79] trigger longer cumulative exposure to two sex hormones (estrogen and progesterone).[38] The higher release of estrogen (exposure to estradiol) as a young adult is thought to influence risk[80] through increased estrogen-dependent diseases such as endometriosis.[31] In addition, early menarcheal age is related to more menstrual cycles, which may increase the possibility of disease initiation.
Results from Arumugam and Lim’s[51] review demonstrate about the salient features concerning the feminine qualities like early onset of fewer than 12 years and short period lengths might expand the openness of the peritoneal hole to a retrograde monthly cycle, building the gamble of creating endometriosis.[58] The report of the meta-analysis is further corroborated by the recent findings[31] that the reflection of early menarcheal age on more response to bleeding (exposure to menstruation) potentiates the function of hormonal milieu and inflammation in developing metabolic outcome (the pathogenesis of endometriosis).
From the results (in a meta-analysis) of the in-depth review on disaggregated data across the globe totaling cases of 3805 (18 case-control studies involving 3805 cases) versus 9526 controls, Nnoaham et al. found the evidence-based mild risk of endometriosis-related early menarche (<12-years-old)[81] seemingly present in low-income countries. This was found in another systemic review but is subject to warranting population-based design (a large cohort study),[82] which found this trend to be higher in their meta-analysis study.[83]
Early menarche could be indicative of associated menstrual abnormality that might involve patients (may be predisposed women) afflicted with endometriosis through retrograde menstruation[77] as reported by hitherto reports (number of studies) but having less number of subjects (small sample size) sometimes devoid of significant linear trend.[38,39,49,50,53,58] On the contrary, a linear association between menarche and laparoscopically confirmed endometriosis (P test for trend 0.001) is found in the Nurses’ Health Study,[38] but is not confirmed from one study of Heilier et al.,[42] despite the involvement of risk factor between 12.5 ([OR] odds ratio) [OR] 0.86, 95% confidence interval [CI] [0.86, 95% CI] 0.68, 1.10) in deep endometriotic nodules and 13 (OR 1.0, 95% CI 0.84, 1.28) of menarcheal age.[42]
Apropos the causal role of the advanced maturation (≤11–>11) and the exposure to the disease (incidence of endometriosis), one study Hemmings et al.[43] met with an interesting observation. The association is found to be significant from a single cohort but is not there from the findings of three surgical (diagnostic laparoscopy, tubal ligation, and hysterectomy) categories. Another study Mamdouh et al.[36] positively demonstrated the trend on women afflicted with endometriosis experiencing maturation (purported to be [defined as] 11 years) (OR = 2.2; 95% CI 1.19–4.22) (P < 0.05). This result was supported by earlier observations linking endometriosis risk to early menarche.[40] Other workers failed to confirm the causal relation with (the association between early menarche and) the endometriosis.[43] Incidentally, one study Treloar et al.[40] found surgically (that women with laparoscopically) diagnosed endometriosis closed proximity to the pubertal beginning of the onset of period (with early menarche) (OR = 0.3; 95% CI 0.1–0.6) seems plausible to develop endometriosis.
One study Kvaskoff et al.[46] confirmed the results favoring disease probability (reported associations between endometriosis risk and earlier menarcheal age) as a potentially identified novel endometriosis predictor among exposures occurring in childhood or adolescence. Hence, this study[46] warranted further research to unfold an allied complexity (the underlying mechanisms) for endometriosis. Using fertile controls, multivariate analysis uncovered a weak outcome (association between age at menarche) between ≤11 (OR = 1.4; 95% CI 0.5–4.6) and ≥13 (OR = 1.1; 95% CI 0.4–2.8) years and endometriosis. When the analysis was repeated with the infertile control group under ≤11 (OR = 2.2; 95% CI 0.5–9.2) and ≥13 years (OR = 1.0; 95% CI 0.4– 2.6), this relationship became somewhat stronger but did not meet significance level. This makes a valid argument for the relevance of putative factors of menstrual cyclicity as possible markers of developing endometriosis had come out from a previous study.[39] On the contrary, such an evidence-based confirmation allows to be refuted by earlier study using control group having an inclusion criteria of sub-fertility is not associated with endometriosis.[53]
Normative menarche
The normative menstrual bleeding in (age at menarche of) 12–13 years is said to cause endometriosis risk. Partial support was demonstrated for the second hypothesis, which conforms to the evidence-based studies. Mahmood and Templeton [Figure 1] found a significant association (<0.05) of disease propensity having an average range, for instance, 12.54 ± 1.53 years in the endometriosis group (n = 227) and 13.07 ± 1.58 years in the no endometriosis group (n = 1315).[84] In another outcome work retrieving 1282 sub-fertile women from the recorded history (retrospective study of 1282 surgical patients in an infertility institute) in Iran- based hospital within the range from 2011 to 2013[85] [Figure 2], identified sub-fertile patients (n = 341) diagnosed condition under study with a mean age at menarche of 13.1 ± 1.2 years, along with having sub-fertility (n = 332) (control) with a mean age at menarche of 13.1 ± 1.3 years devoid of pelvic inflammatory disease.
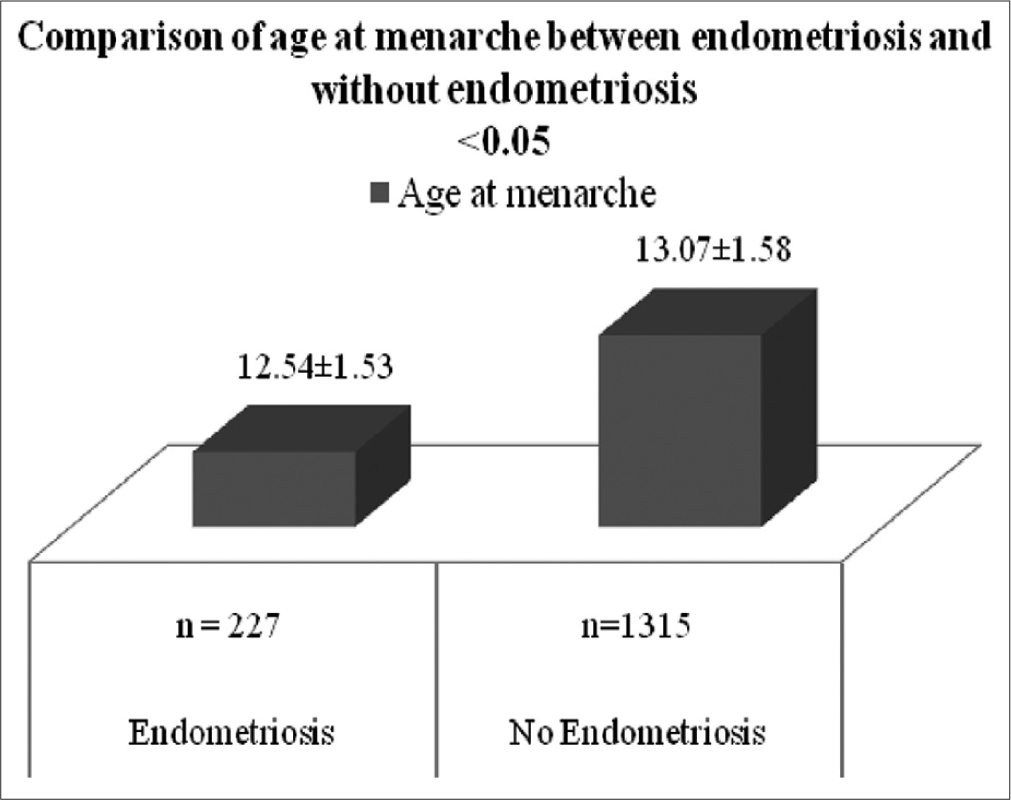
- Comparison of age at menarche between endometriosis and without endometriosis.
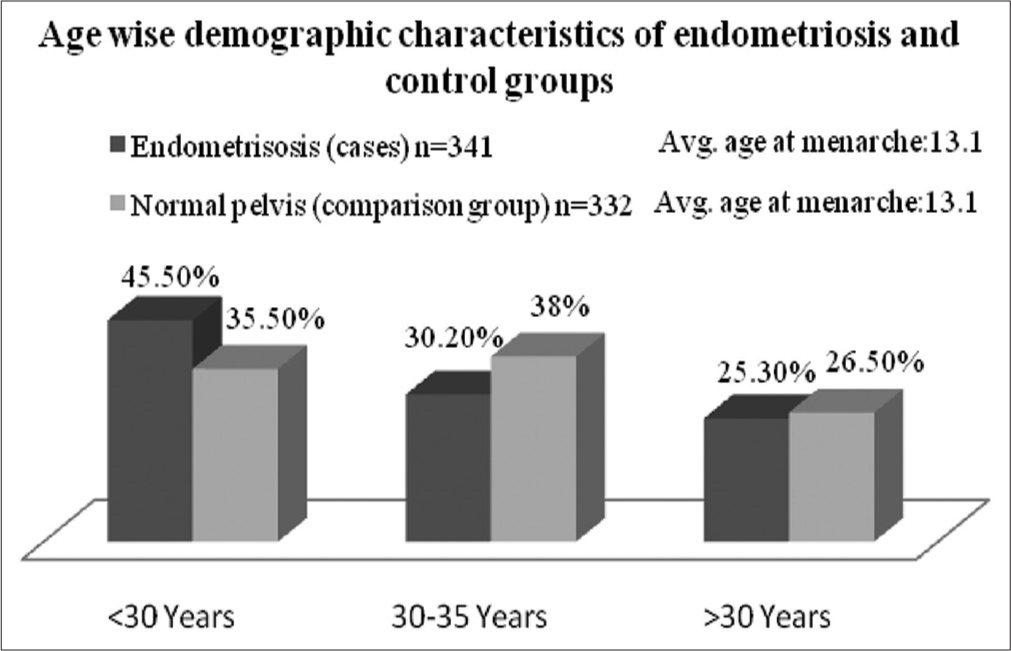
- Age-wise demographic characteristics of case and comparison groups.
Late menarche
Women who have endometriosis have variable ages at menarche, ranging from early to normative, and late studies provided partially support third hypothesis. The findings did document that both Lombardy[49] [Figure 3] and Oxford Endometriosis Gene[63] studies demonstrated the involvement of early, normative, and late menarcheal age (11–14 years) with endometriosis. Study investigators had further used the rASRM protocol of categorizing disease (classification of endometriosis) (1996) to show different stages of early (stages I and II) and late (stages III and IV) disease stages [Figure 3].[86] In a large population-based investigation (prospective cohort study), Japan Nurses’ Health Study (JNHS), there was a significant trend towards higher probability of disease (increased risk of endometriosis) present not only at the younger age of menarche (≤11) in diagnosed (surgically confirmed endometriosis) groups (n = 210) but also such risk persisted in other menarcheal ages of 12, 13, and 14 years in the same group.[87]
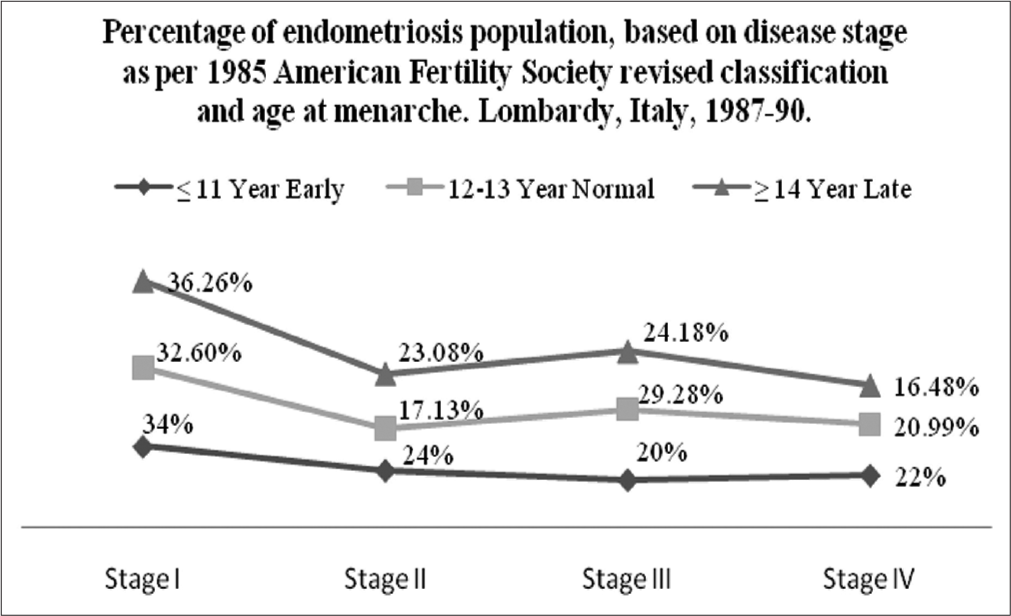
- Percentage of endometriosis, based on disease stage and age at menarche.
Late menarche is inversely related with (associated with the subsequent risk of) endometriosis (OR = 0.3; 95% CI 0.1–0.6), found in an evidence-based study.[40] Nevertheless, late menarche is supposed to be a guiding principle to workout both the investigation including treatment (diagnostic and therapeutic) strategy to corroborate the related symptoms warranting endometriosis. The said study[40] found a significantly decreased chances at later age (≥14 years at menarche) but with a limited clinical findings against the reduced risk associated with the later stage of onset. On the contrary, age at menarche under ≥14 years can be the tool facilitating the (to guide diagnostic and therapeutic) strategy, which provided when allied complications (if any other symptoms) suggest favoring possible outcome (endometriosis as a possible diagnosis).
MENARCHEAL AGE IS NOT IN THE ETIOLOGIC PATHWAY TO ENDOMETRIOSIS
Exposure to the menstruation seems plausible to be not related to develop disease at (women diagnosed with endometriosis) later in life. The following studies are in a position to support this hypothesis. Having probed the putative causes related to cyclicity (while describing the menstrual profile [age at menarche]) [Figure 4] in determining about its ubiquity (the prevalence of endometriosis) between the surgically confirmed Puerto Rican women (n = 57) and general women (n = 1228) population with no endometriosis in Puerto Rico in the Caribbean island. Flores et al.[34] reported that although this estrogen caused disorder is not severe ailment present in the said Caribbean island, showing the highest percentage (42.10%) [Figure 4] of diseased prone patients (of women with endometriosis) in 12–13 groups of women (age at menarche compared) to their very early and late counterparts. It seems plausible that menstrual characteristics had hardly any impact on endometriosis.[34]
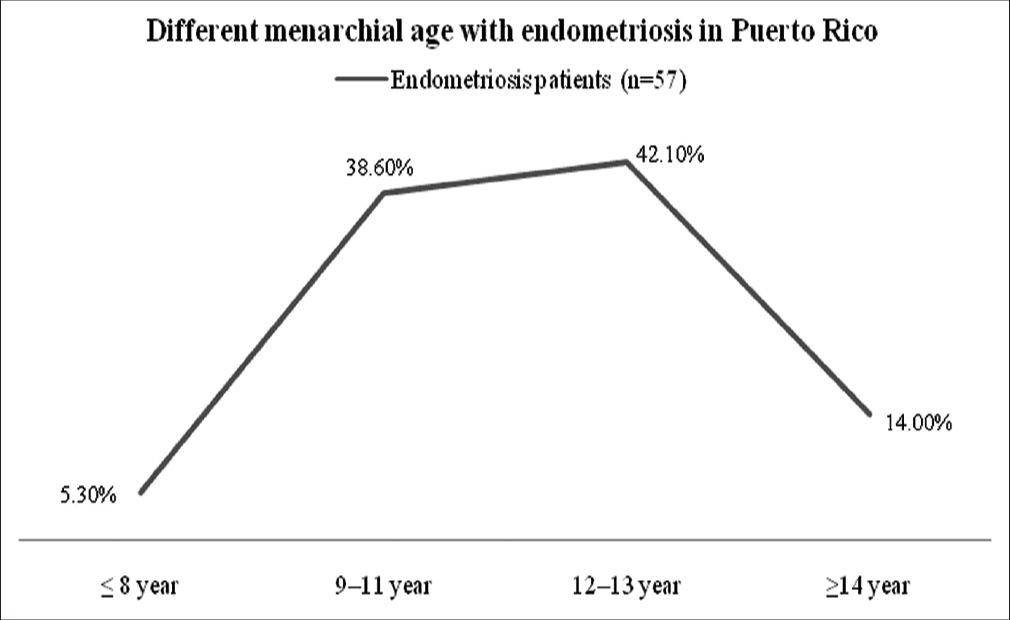
- Different menarcheal age with endometriosis in Puerto Rico.
Percentage in regard to the diagnosed patients (all of them belong to stage III–IV) by revised criteria of the rASRM[86] pertinent to the incident cases in a prospective matched study reported more reproductive ailments (pelvic pain or dysmenorrhea) in the past year of three categories of menarcheal age [Figure 5] of ≤11 years = 37 (19.9%), 12–13 years = 87 (46.8%), and ≥14 years = 62 (33.3%) in operative cohort of n = 473 compared to ≤11 years = 2 (15.4), 12–13 years = 5 (38.5), and ≥14 years = 6 (46.2) in population cohort of n = 127 having mean±Standard Deviation of 13.0±1.8 years and 13.2±1.5 years, respectively.[59] Hence, three categories of menarcheal age, along with or without a pedigree depicting the inheritance pattern of disease (family history of endometriosis) are susceptible to endometriosis[55] but independent of drawing inferences from the etiologic pathway. However, asymptomatic estrogen-dependent fact appears to be the stumbling block in assessing the actual span of reproductive disorder (of the disease), thereby delaying diagnosis and eventually facing in fertility treatment.[59]
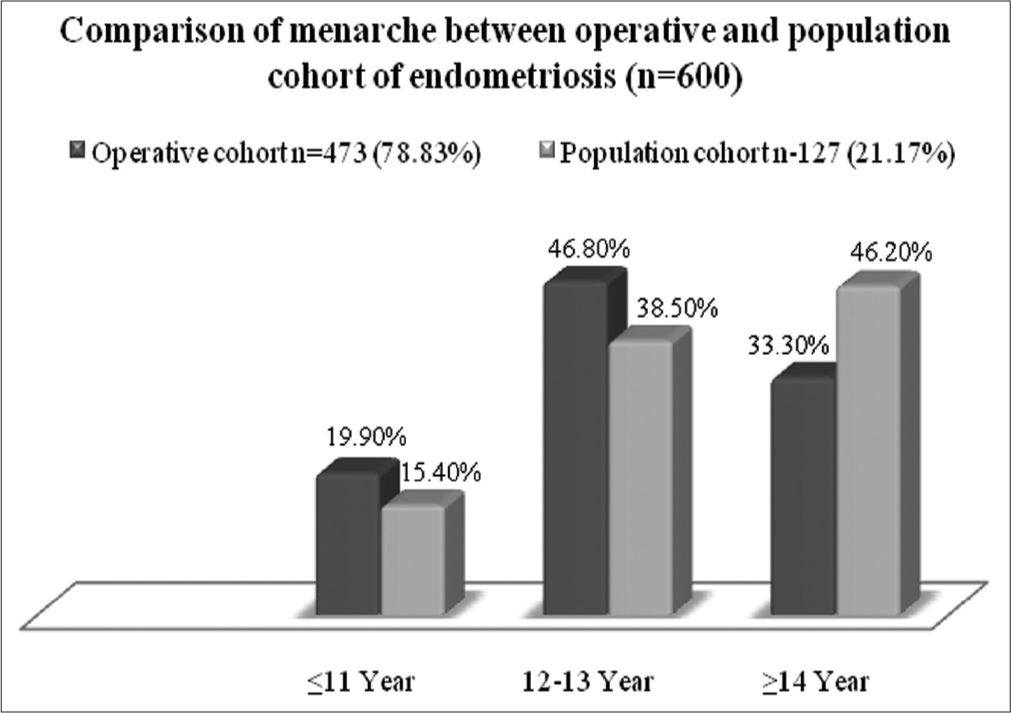
- Different menarcheal age with endometriosis.
A well-design case–control study on Iranian infertile women diagnosed with pelvic endometriosis, Moini et al.[88] reported that the menstrual pattern and amount of menstrual bleeding were significantly different among the control (n = 153), stage I/II (n = 52 and n = 70) along with (n = 122), and stage III/IV (n = 128) groups (P < 0.05), but not to the speak of time of onset of periods pertinent to 13.42 years in control, 13.62 years in early including (stage I/II), and 13.22 years in late as per rASRM classification (in stage III/IV) and dysmenorrhea.[88] The above findings reveal that menarche at 13.42 and 13.22 increases a woman’s risk for endometriosis in later years.
DISCUSSION
The present study makes an exhaustive effort after having assessed the published works in the context of differential time of pubertal maturation caused disease relationship that offers both quantitative and qualitative argument to systematically deal with the underlying reality involving (the effect of) menarche may precede an exposure to the higher level of estrogen response (against the risk of endometriosis) by not ignoring the putative factors of other menstrual characteristics are alluded to almost all the literature under study. The given case-control studies retrieved from the number of published works (in the meta-analysis)[89] on pathogenesis of endometriosis in the early and late stage as laid down in the rASRM classification are carefully interpreted about the direct and indirect role of non-modifiable risk factors[41] rather than analyzing evidence-based and other modifiable risk factors[36] including delay in diagnosis, infertility, lifestyle, physical activities,[39] and environmental exposure[42] along with pelvic abnormality.[39] Further, identifying menstrual and allied characteristics are stupendous exercise from symptoms of progressive and multicausal[42] endometriosis, due to have long span within (a range of) 10–19 year age.[40]
Most of these results have, however, been based on small sample size,[42] which are devoid of a linear trend,[54] that bars obtaining comprehensive results on clinical plausibility,[36] thereby facing obstruction in enrolling cases, since significant linear trend may not always be found.[40] Furthermore, studies with low statistical power, poorly defined study populations, and inadequate adjustment for confounders may cause hindrance of revealing the results.[90] Kvaskoff et al.[46] claimed a kind of limitation in their study design is due to the long time-frame happens between the studied exposures and disease occurrence that poses a question of reliability of data on infertility against controls by virtue of differences in risk profiles. Much later, a remark from (one study in) Sweden[54] met with some limitations by virtue of the cross-sectional study, where follow-up was not there after 1ong-time collection of information that may affect disease legitimacy in the population. Another study Burghaus et al.[47] encountered certain limitations in a hospital-based study that may cause the selection bias of both the disease and healthy cohorts (cases and controls) in influencing results. It could be lesser, had it been a population based.
From hitherto findings of overall menstrual characteristics pertinent to the differential onsets of periods, lending an evidential support attributed to Sampson’s argument on reflux (theory of retrograde) menstruation.[77] It states that menstrual characteristics of women release more menstrual debris covering ectopic cells of outside the uterus (in the peritoneal cavity) is likely to exacerbate (increase the risk of) the progression of endometriosis.[42] It is further exacerbated by longer periods,[43,47] short cycle length,[36,39,43,55,58] irregular cycle,[41,42] and heaviness of flow.[40] This sparks a question regarding the clarity of association between menstrual characteristics[44] and endometriosis[39] that may not support an intricacy concerning (the association between) the overarching cyclicity (age at menarche) per se and endometriosis.[38] The present study has been dealt with an array of comprehensiveness for (the impact of) the prognostication of disease (exposure to menstruation) met with limitation for not addressing any causality regarding (the effect of) menstrual characteristics other than periodical anomalies[91] (age at menarche).
CONCLUSION
Before confirming a significant relation with endometriosis, the evidence-based details from the above four hypotheses state that menarche matters to make (is involved in the) initiation related to the pathogenesis (of the disease) directly or indirectly and is unique for its relevance from the onset to developing (diagnosis of the) disease at eventual circumstances in (the onset of the onset of) menstrual life at about the age of <11 years. A girl who has endometriosis either in her adolescence or in her early or mid-20’s has no symptom or symptom of pain or a cascade played at the arrhythmic monthly cycle (of menstrual irregularities). Concurrent pain and other irregularities may be the symptoms that are kept unnoticed by the patient for a longer duration. However, early menarche matches with certain probabilities, (as a risk factor) offers several conclusions postulated in numerous studies, including the possibility of endometriosis.
Onset of puberty ushers in a sexual maturity of woman (Menarche is defined as the first menstrual period in a female adolescent). It happens in early teens with a mean within the range of 12.4 (menarche typically occurs between the ages of 10 and 16, with the average age of onset being 12.4) years is not abstaining to exposure to (from the risk of) endometriosis found in studies? By the proximal end of the early menarche category, it is unclear whether these groups behave as early menarche groups. Mahmood and Templeton’s remark about a “younger group” resonates with this proximity. When preponderance found in (the risk of) endometriosis persists in the early, normative, and late menarche groups, plausibility toward the (the risk of) disease prevalence in advance sexual maturity is (early menarche has) failed to be understood. Nevertheless, the secular trend of early maturation, with evidence of the growing impact on (prevalence of endometriosis in) developed countries and the early age of menarche less then equal of the age of 12 years (as ≤12 years) by some authors, is tantamount to the involvement of menarche in developing the disease.
There is no denying that the great deal of dearth of appropriate clinical markers and pathognomonic signs, it is difficult to locate the endometriosis spot before a confirmed diagnosis. Hence, clinical markers are paramount to facilitating the earlier endometriosis diagnosis.
Ethical approval
The Institutional review board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Brief communication: Menarche is related to fat distribution. Am J Phys Anthropol. 2007;133:1147-51.
- [CrossRef] [PubMed] [Google Scholar]
- International variability of ages at menarche and menopause: Patterns and main determinants. Hum Biol. 2001;73:271-90.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution, development and timing of puberty. Trends Endocrinol Metab. 2006;17:7-12.
- [CrossRef] [PubMed] [Google Scholar]
- Worldwide variation in human growth Cambridge: Cambridge University Press; 1991. p. :1-397.
- [CrossRef] [Google Scholar]
- Environmental factors and puberty timing: Expert panel research needs. Pediatrics. 2008;121:S192-207.
- [CrossRef] [PubMed] [Google Scholar]
- The menstrual cycle in a biopsychosocial context In: Denmark FL, Paludi MA, eds. Psychology of women: A handbook of issues and theories. United States: Praeger Publishers; 2008. p. :400-39.
- [CrossRef] [Google Scholar]
- Early and late menarche and risk of depressive symptoms in young adulthood. Arch Womens Ment Health. 2014;17:511-8.
- [CrossRef] [PubMed] [Google Scholar]
- Relation of early menarche to depression, eating disorders, substance abuse, and comorbid psychopathology among adolescent girls. Dev Psychol. 2001;37:608-19.
- [CrossRef] [PubMed] [Google Scholar]
- Critical psychophysical passages in the life of substance abuse, and comorbid psychopathology among adolescent girls. Dev Psychol. 2001;37:608-19.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual cosmology among the Beng of Ivory Coast In: Buckley T, Gottlieb A, eds. Early blood magic: The anthropology of menstruation. Berkeley: University of California Press; 1988. p. :55-74.
- [CrossRef] [Google Scholar]
- Menstrual symptoms: The importance of social factors in women's experiences. Br J Gen Pract. 2006;56:950-7.
- [Google Scholar]
- Special issue: Blood mysteries: Beyond menstruation as pollution. Ethnology. 2002;41:381-90.
- [Google Scholar]
- A critical appraisal of theories of menstrual symbolism In: Blood magic: The anthropology of menstruation. Berkeley: University of California Press (US); 1988. p. :3-12.
- [CrossRef] [Google Scholar]
- Male power and menstrual etiquette In: Thomas H, ed. The sexual politics of reproduction. United Kingdom: Gower Publication; 1985.
- [Google Scholar]
- Age at menarche and secular trend in Maharashtrian (Indian) girls. Acta Biol Szeged. 2000;44:53-7.
- [Google Scholar]
- Study of age at menarche, the secular trend and factors associated with it. Internet J Biol Anthropol. 2008;2:1-7.
- [Google Scholar]
- Age at menarche in girls and the developmental origin of health and diseases. Ann Agric Environ Med. 2012;19:883-7.
- [Google Scholar]
- Secular changes in human biological variables in Western countries: An updated review and synthesis. J Anthropol Sci. 2008;86:91-112.
- [Google Scholar]
- The oestrogen receptor alpha gene is linked and/or associated with age of menarche in different ethnic groups. J Med Genet. 2005;42:796-800.
- [CrossRef] [PubMed] [Google Scholar]
- Age at natural menopause and sociodemographic status in Finland. Am J Epidemiol. 1994;139:64-76.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive and general lifestyle determinants of age at menopause. Maturitas. 1992;15:141-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nutritional status and age at menarche of Senegalese adolescents. Ann Hum Biol. 1997;24:521-32.
- [CrossRef] [PubMed] [Google Scholar]
- Season of birth and recalled age at menarche. J Biosoc Sci. 1992;24:167-73.
- [CrossRef] [PubMed] [Google Scholar]
- Body weight and the initiation of puberty. Clin Obstet Gynecol. 1985;28:573-9.
- [CrossRef] [PubMed] [Google Scholar]
- Ages at menopause and menarche in a high-altitude Himalayan population. Ann Hum Biol. 1983;10:365-70.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of high altitude on age at menarche and menopause. Int J Biometeorol. 1986;30:21-6.
- [CrossRef] [PubMed] [Google Scholar]
- Energy economy in the evolution of menstruation. Evol Anthropol. 1996;5:157-64.
- [CrossRef] [Google Scholar]
- The evolution of endometrial cycles and menstruation. Q Rev Biol. 1996;71:181-220.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual cycling and breast cancer: An evolutionary perspective. J Womens Health. 1999;8:193-202.
- [CrossRef] [PubMed] [Google Scholar]
- Comfortable with their bodies: Menstruation, culture and materialism in America [Thesis] 2012. Georgia: Georgia State University; Available from: https://scholarworks.gsu.edu/anthro_hontheses/8 [Last accessed on 2022 Jul 12]
- [Google Scholar]
- Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. 2017;209:3-7.
- [CrossRef] [PubMed] [Google Scholar]
- Endocrine characteristics of adolescent menstrual cycles: Impact of early menarche. J Steroid Biochem. 1984;20:231-6.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual and reproductive factors in relation to ovarian cancer risk. Br J Cancer. 2001;84:714-21.
- [CrossRef] [PubMed] [Google Scholar]
- Self-reported prevalence of endometriosis and its symptoms among Puerto Rican women. Int J Gynaecol Obstet. 2008;100:257-61.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal pre-pregnancy BMI, gestational weight gain, and age at menarche in daughters. Matern Child Health J. 2013;17:1391-8.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic determinants of endometriosis among Egyptian women: A hospital-based case-control study. J Egypt Public Health Assoc. 2011;86:21-6.
- [CrossRef] [PubMed] [Google Scholar]
- Growth at adolescence: With a general consideration of the effects of hereditary and environmental factors upon growth and maturation from birth to maturity United Kingdom: Blackwell Scientific Publications; 1962.
- [Google Scholar]
- Reproductive history and endometriosis among premenopausal women. Obstet Gynecol. 2004;104:965-74.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiologic determinants of endometriosis: A hospital-based case-control study. Ann Epidemiol. 1997;7:267-741.
- [CrossRef] [PubMed] [Google Scholar]
- Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am J Obstet Gynecol. 2010;202:6.e1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Early menarche, a risk factor for breast cancer, indicates early onset of ovulatory cycles. J Clin Endocrinol Metab. 1983;57:82-6.
- [CrossRef] [PubMed] [Google Scholar]
- Environmental and host-associated risk factors in endometriosis and deep endometriotic nodules: A matched case-control study. Environ Res. 2007;103:121-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of risk factors associated with endometriosis. Fertil Steril. 2004;81:1513-21.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics related to the prevalence of minimal or mild endometriosis in infertile women. Canadian Collaborative Group on Endometriosis. Epidemiology. 1998;9:504-10.
- [CrossRef] [PubMed] [Google Scholar]
- Age at menarche does not correlate with the endometriosis phenotype. PLoS One. 2019;14:e0219497.
- [CrossRef] [PubMed] [Google Scholar]
- Childhood and adolescent exposures and the risk of endometriosis. Epidemiology. 2013;24:261-9.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for endometriosis in a German case-control study. Geburtshilfe Frauenheilkd. 2011;71:1073-9.
- [CrossRef] [PubMed] [Google Scholar]
- Association between sexual activity during menstruation and endometriosis: A case-control study. Int J Fertil Steril. 2019;13:230-5.
- [CrossRef] [Google Scholar]
- Pelvic endometriosis: Reproductive and menstrual risk factors at different stages in Lombardy, northern Italy. J Epidemiol Community Health. 1995;49:61-4.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive and menstrual factors and risk of peritoneal and ovarian endometriosis. Fertil Steril. 1991;56:230-4.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual characteristics associated with endometriosis. Br J Obstet Gynaecol. 1997;104:948-50.
- [CrossRef] [PubMed] [Google Scholar]
- Age at menarche, duration of monthly flow and cycle length as risk factors for endometriosis in Sub-Sahara Black African women. Pregn Womens Health Care Int J. 2021;1:1-12.
- [CrossRef] [Google Scholar]
- Epidemiology of endometriosis in infertile women. Fertil Steril. 1995;63:34-8.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive and lifestyle factors associated with endometriosis in a large cross-sectional population sample. J Womens Health (Larchmt). 2017;26:152-8.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological characteristics in women with and without endometriosis in the Yale series. Arch Gynecol Obstet. 2008;277:389-93.
- [CrossRef] [PubMed] [Google Scholar]
- Intrauterine exposures and risk of endometriosis. Hum Reprod. 2007;22:3232-6.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual cycle characteristics and the risk of endometriosis. Epidemiology. 1993;4:135-42.
- [CrossRef] [PubMed] [Google Scholar]
- The relation of endometriosis to menstrual characteristics, smoking, and exercise. JAMA. 1986;255:1904-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors associated with endometriosis: Importance of study population for characterizing disease in the ENDO Study. Am J Obstet Gynecol. 2013;208:11.e1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Adenomyosis and endometriosis in the California teachers study. Fertil Steril. 2008;90:415-24.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual symptoms in women with pelvic endometriosis. Br J Obstet Gynaecol. 1991;98:558-63.
- [CrossRef] [PubMed] [Google Scholar]
- Study on epidemiology of endometriosis in North East India. Int J Reprod Contracept Obstet Gynecol. 2023;12:1770-4.
- [CrossRef] [Google Scholar]
- Differences in characteristics among 1,000 women with endometriosis based on extent of disease. Fertil Steril. 2008;89:538-45.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers in endometriosis: Challenges and opportunities. Fertil Steril. 2017;107:523-32.
- [CrossRef] [PubMed] [Google Scholar]
- Menarche: A missing indicator in population health from low-income countries. Public Health Rep. 2013;128:399-401.
- [CrossRef] [PubMed] [Google Scholar]
- Adolescent reproductive health challenges among schoolgirls in southeast Nigeria: Role of knowledge of menstrual pattern and contraceptive adherence. Patient Prefer Adherence. 2015;9:1219-24.
- [CrossRef] [PubMed] [Google Scholar]
- The timing of normal puberty and the age limits of sexual precocity: Variations around the world, secular trends, and changes after migration. Endocr Rev. 2003;24:668-93.
- [CrossRef] [PubMed] [Google Scholar]
- Association between adolescent idiopathic scoliosis prevalence and age at menarche in different geographic latitudes. Scoliosis. 2006;1:9.
- [CrossRef] [PubMed] [Google Scholar]
- Age at menarche, total mortality and mortality from ischaemic heart disease and stroke: The Adventist Health Study, 1976-88. Int J Epidemiol. 2009;38:245-52.
- [CrossRef] [PubMed] [Google Scholar]
- When little girls become women: Early onset of puberty in girls. 2001. The Ribbon. :6. Available from: https://www.timeenoughforlove.org/saved/girlsbecomewomen.htm [Last accessed on 2019 Nov 22]
- [Google Scholar]
- Effect of low versus normal birth-weight on menarche in 14-year-old Polish girls. J Paediatr Child Health. 2002;38:268-71.
- [CrossRef] [PubMed] [Google Scholar]
- Secular trends in the anthropometry of adolescents and college students: Polish perspective In: Preedy VR, ed. Handbook of anthropometry: Physical measures of human form in health and disease. United States: Springer-Verlag; 2012. p. :1-1330.
- [CrossRef] [Google Scholar]
- High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094-101.
- [CrossRef] [PubMed] [Google Scholar]
- Transposable elements: Targets for early nutritional effects on epigenetic gene regulation. Mol Cell Biol. 2003;23:5293-300.
- [CrossRef] [PubMed] [Google Scholar]
- Is female health cyclical? Evolutionary perspectives on menstruation. Trends Ecol Evol. 2018;33:399-414.
- [CrossRef] [PubMed] [Google Scholar]
- Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol. 2018;33:399-414.
- [Google Scholar]
- Endometriosis: Ancient disease, ancient treatments. Fertil Steril. 2012;98:S1-62.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of endometriosis. Obstet Gynecol Clin North Am. 1997;24:235-58.
- [CrossRef] [PubMed] [Google Scholar]
- Earlier menarche is associated with lower insulin sensitivity and increased adiposity in young adult women. PLoS One. 2015;10:e0128427.
- [CrossRef] [PubMed] [Google Scholar]
- Is early age at menarche a risk factor for endometriosis? A systematic review and meta-analysis of case-control studies. Fertil Steril. 2012;98:702-12.e6.
- [CrossRef] [PubMed] [Google Scholar]
- Association between early menarche and endometriosis risk: A systematic review and meta-analysis. Authorea 2020:1-22.
- [CrossRef] [Google Scholar]
- The risk of endometriosis by early menarche is recently increased: A meta-analysis of literature published from 2000 to 2020. Arch Gynecol Obstet. 2023;307:59-69.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and genesis of endometriosis. Hum Reprod. 1991;6:544-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of risk factors associated with endometriosis in infertile women. Int J Fertil Steril. 2016;10:11-21.
- [Google Scholar]
- Risk profiles for endometriosis in Japanese women: Results from a repeated survey of self-reports. J Epidemiol. 2015;25:194-203.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors associated with endometriosis among infertile Iranian women. Arch Med Sci. 2013;9:506-14.
- [CrossRef] [PubMed] [Google Scholar]
- Factors and regional differences associated with endometriosis: A multi-country, case-control study. Adv Ther. 2016;33:1385-407.
- [CrossRef] [PubMed] [Google Scholar]
- What makes a good case-control study? Design issues for complex traits such as endometriosis. Hum Reprod. 2002;17:1415-23.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual cycle among adolescents: Girls' awareness and influence of age at menarche and overweight. Rev Paul Pediatr. 2022;40:e2020494.
- [CrossRef] [PubMed] [Google Scholar]







